Spine Fusion Epidemic: Why More Surgery Means Worse Outcomes
As a surgeon who has dedicated my career to fixing failed back surgeries and offering a real alternative to the medieval practice of spinal fusion, I have a front-row seat to the catastrophe unfolding in modern spine care. What I see is a betrayal of patient trust on a massive, industrial scale, driven not by medical necessity, but by a relentless pursuit of profit.
I want to be perfectly clear: the exponential rise in spinal fusion surgery is not a medical breakthrough. It is an economic phenomenon. It is a calculated response to financial incentives that reward invasiveness and complexity. At the same time, the patient, the supposed beneficiary, suffers the collateral damage of a system that is sacrificing ethics for enrichment.
The Fusion Explosion: An Unprecedented Rise in Spinal Surgery
If you rewind the clock to the 1980s and early 1990s, you’ll see a different era. Spinal fusion was a rare procedure. Back then, somewhere around fewer than 1% of spine surgeries involved fusing vertebrae. Surgeons performed mostly laminectomies and discectomies, invasive procedures that relieved nerve compression without permanently locking the spine in place.
Fast forward three decades. The landscape is unrecognizable. The incidence of spinal fusion rates has skyrocketed from fewer than 40,000 procedures annually to close to a million a year. That is a 20-fold increase in 30 years.
Let that sink in. A surgical procedure that was once a last resort for catastrophic spinal instability is now performed close to a million times a year, often for routine back pain or degenerative disc conditions where non-fusion alternatives are proven effective.
What has driven this astonishing change? It is not an epidemic of new spine conditions. The increased rates in spinal fusion surgeries a perfect storm of three financially incentivized entities: the medical device companies, the surgeons, and the hospitals.
The Role of Spinal Device Companies: Engineering Demand
The primary driver of this fusion epidemic is the medical device and implant industry. These companies are generating billions upon billions of dollars in profit from spinal fusions.
Every fusion requires a laundry list of expensive, patented devices and medications:
- Interbody cages
- Screws
- Rods
- Metal plates and cross-links
- Biologics (biologically active substances that assist the fusion process)
The devices, specifically the spinal implants, are often the primary component of surgical supply costs, sometimes accounting for nearly 85% of the direct cost of the procedure.

The Sales Rep Network and Ethical Compromise
These companies have created a pervasive network of influence, spearheaded by their sales representatives. Rather than selling equipment; they are selling a procedure. They are going to hospitals, meeting with surgeons, and taking them out for lunch, dinner, and drinks—whatever it takes to ensure that the surgeon is using that company's devices or biologics.
An Uncensored Look
Watch Dr. Deukmedjian explain this corrupt dynamic in "Spine Scam, Official Trailer."
Infiltration of Education and Thought Leadership
The implant companies' influence reaches beyond the operating room. They have systematically infiltrated the educational system at major university training centers. They develop deep financial relationships with spine industry thought leaders, including professors and department chairmen, thereby influencing the people who train the next generation of surgeons.
These professors and leaders receive substantial stipends, consulting fees, and royalty arrangements. In return, they teach residents and fellows to perform spinal fusions, often with an emphasis on the very devices produced by the companies that pay them. This cycle ensures that the most lucrative procedures become the standard of care for new surgeons, regardless of the clinical data.
As a result of these relationships, the next generation of doctors is taught that complex, instrumented fusion is the best option, further cementing the practice and the profits of the device companies
The Surgeon's Wallet: Financial Incentives That Betray Trust
When a patient seeks treatment for chronic back or neck pain, they put their absolute trust in their doctor to recommend the best, safest, and most effective treatment. This is a sacred relationship. Unfortunately, in the spine industry, that trust is often betrayed by the sheer magnetic pull of financial gain.
The core issue lies in the system of reimbursement. Look at the payment structure for a surgeon:
- Discectomy: Around $500.
- Laminectomy: Around $800.
- Spinal fusion (complex): Anywhere between $10,000 and $20,000.
When you compare the surgeon's pay, the financial incentive to perform a spinal fusion is 20 times higher than for the types of surgeries we used to perform. Complex spinal fusions represent some of the highest payments to doctors in medicine for any single treatment. Spine surgeons have become increasingly incentivized to perform the most invasive, complicated, and expensive procedure (a fusion) over simpler, less invasive options.
This isn't just about a higher fee for more complex work. Studies have investigated the relative reimbursement rates for isolated decompression versus decompression and instrumented fusion. While some literature attempts to defend the current payment structure, arguing that the increased time and effort for a fusion procedure does not always translate to a higher dollar per minute of a surgeon’s time, the undeniable reality is that the volume of high-reimbursement procedures has surged. Spine surgeons are financial gatekeepers, and when the gate to a $20,000 procedure is always open, patient volume and procedural complexity inevitably rise.
The system tends to prioritize invasiveness, resulting in a focus on surgical volume over patient value.
Hospitals: The Silent Partner in the Fusion Profit Machine
The third powerful force driving the fusion epidemic is the hospital system itself. Hospitals make more money and a higher profit margin from spinal fusion surgery than from almost any other procedure they perform.
A single spinal fusion surgery can generate between $50,000 and $500,000 in payments to the hospital for the surgery, stay, associated services and complications addressed down the road. Naturally, hospitals are highly incentivized to increase their fusion volume. They actively foster relationships with, and aggressively recruit, spine surgeons who specialize in fusions to ensure their operating rooms are constantly busy with these lucrative procedures.
The combination of massive profits for the surgeon, massive revenue for the implant company, and massive profits for the hospital creates an "industrial complex," a symbiotic financial relationship where all three parties are rewarded handsomely for performing an invasive procedure.
The Patient as Victim: Worsening Outcomes and Lost Trust
The core tragedy of this system is that as the financial rewards for the practitioners, companies, and facilities have increased, the outcomes for the patients have worsened. Patients are now the victims of these financial forces.
While proponents of fusion surgery sometimes claim improved long-term outcomes for pain control, the body of high-quality, peer-reviewed literature reveals a more sobering reality.
High Complication and Reoperation Rates
Spinal fusion is a major, highly invasive surgery, and the risk of complications is significant. The postoperative complication rates for spinal fusion can range from 8.6% to 49.1%, with many studies suggesting the true incidence is between 15% and 25%.
Even more concerning is the long-term prognosis. Many patients continue to suffer from chronic pain years after the surgery. A significant number of patients undergoing fusion will require additional procedures down the road, with some studies showing a substantial reoperation rate due to complications.
For more information on the risks you face, read some of the facts in the following blogs:
The Inevitability of Adjacent Segment Disease (ASD)
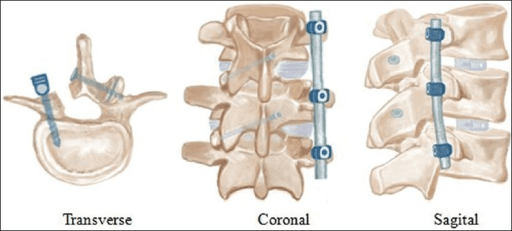
One of the most devastating long-term effects of spinal fusion is a condition known as Adjacent Segment Disease (ASD). When you fuse two or more vertebrae together with metal rods and screws, you eliminate all movement at the fused segment. That movement—that biomechanical stress—doesn't disappear; it is transferred to the discs immediately above and below the fused segment.
Over time, this increased stress causes the adjacent discs to degenerate rapidly, leading to a new herniation, stenosis, or instability that is often worse than the original problem. This frequently necessitates another fusion on the next segment, leading to a downward spiral of pain, surgery, and lost mobility. For a patient, this is a path to becoming a permanent surgical invalid.
We see this repeatedly in different fusion types:
Long-Term Resource Use and Opioid Dependency
The postoperative path for fusion patients is often marked by continuous medical resource utilization, including long-term pain and psychotropic medication. Studies have demonstrated that a majority of patients who underwent lumbar fusion continued chronic narcotic use two years post-surgery. Furthermore, chronic opioid use before surgery has been linked to an increased risk of complications, re-admission, and repeat spinal surgery, highlighting a vicious cycle of failed treatment.
The system has become a machine that generates surgical volume, device profits, and, tragically, a large population of patients who are doing worse than ever before, trapped in a cycle of pain management and potential reoperation.
Reclaiming Spine Care: A Surgeon’s Responsibility
The primary drivers of the spinal fusion surge—the implant companies' pervasive influence, the surgeons' financial incentives, and the hospitals' drive for maximum revenue—have clouded clinical judgment and corrupted the patient-doctor relationship.
It is time to acknowledge the overwhelming evidence that for many common spine conditions, fusion is simply not the answer. A minimally invasive, non-fusion approach is superior for the vast majority of chronic back pain sufferers. Find more information on how to avoid these disastrous operations and alternative treatment options on the Deuk Spine Institute blog.
The industry must return to a standard of care where the least invasive, most targeted, and most clinically sound procedure is always the first choice.
Curious About How It Works?
Watch an endoscopic disc repair.
The Better Way: Deuk Laser Disc Repair (DLDR)
For patients suffering from debilitating pain or severe instability, the benefits of spinal surgery might seem to outweigh the risks significantly. However, as you can see, they are not procedures without consequences. There is one procedure that has none of these consequences.

My revolutionary procedure, Deuk Laser Disc Repair® (DLDR), provides a safer alternative for alleviating neck or back pain, minimizing the risk of collateral damage by targeting the muscles, nerves, ligaments, tendons, and joints.
