The pain of a chronic lumbar spine condition affects every aspect of your life. Doctors typically recommend PLIF, a highly invasive procedure, for conditions that cause significant instability or nerve compression, such as degenerative disc disease, spondylolisthesis, spinal stenosis, and recurrent herniated discs. Like any major invasive medical procedure, PLIF carries its own risks and potential complications. This article provides a thorough overview of the risks and complications of PLIF.
What Is PLIF Surgery?
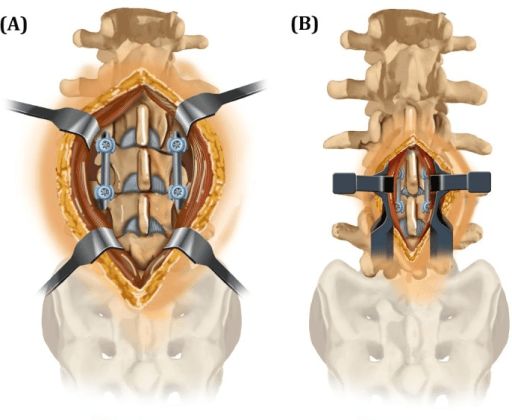
PLIF an invasive spinal fusion surgery used to stabilize the spine and relieve pressure on spinal nerves. The term "posterior" refers to the surgical approach—the surgeon accesses the spine from the back. "Lumbar" indicates the lower back region where the procedure is performed. "Interbody Fusion" describes the main part of the surgery: removing a damaged intervertebral disc and fusing two or more vertebrae using a bone graft or implant.
The Surgical Risks of PLIF Surgery?
The complications related to PLIF surgery can be divided into three main categories: those that happen during the surgery, those that occur shortly after surgery, and those that may develop over the long term.
Surgical Risks
These are risks that can happen in the operating room during the procedure itself. During PLIF surgery, specific muscles, ligaments, and tissues are affected as part of the surgical process.
- Muscle Damage: PLIF surgery may cause muscle damage or, in rare cases, muscle death (also known as muscle necrosis) due to the procedure's impact on surrounding tissues.
- Erector Spinae Muscles: These are the large muscles running along the spine. During PLIF, these muscles are retracted (moved aside) to access the spine. While surgeons aim to minimize damage, some muscle fibers may be affected, leading to post-operative pain and muscle weakness.
- Multifidus Muscle: This deep spinal muscle is often disrupted when approaching the vertebrae. Damage to the multifidus can lead to post-surgical muscle atrophy and decreased spinal stability.
- Ligament Damage:
- Ligamentum Flavum: This ligament, which connects the laminae of adjacent vertebrae, is often removed or partially resected to access the spinal canal and relieve nerve compression.
- Interspinous Ligament: This ligament, located between the spinous processes of neighboring vertebrae, may be cut or removed during surgery.
- Supraspinous Ligament: This ligament runs along the tips of the spinous processes and may also be disrupted during the procedure.
- Soft Tissue Damage:
- Fascia: The thoracolumbar fascia, a connective tissue layer covering the back muscles, is incised to access the deeper structures.
- Subcutaneous Tissue and Skin: The incision through the skin and subcutaneous layers is necessary to reach the spine.
- Other Tissue Damage:
- Intervertebral Disc: The damaged or degenerated disc is removed entirely during the procedure. This is a key part of the surgery, as the disc space is then filled with a bone graft or implant to facilitate fusion.
- Facet Joint Capsule: The capsule surrounding the facet joints may be disrupted or removed, especially if the joints are contributing to nerve compression or instability.
- Nerve Damage: The lumbar spine is a complex network of nerves. Despite the use of advanced monitoring techniques, there is a small risk of damaging the spinal nerves or the dura mater (the protective sac surrounding them). This can lead to new or worsened weakness, numbness, pain, or, in rare cases, loss of bowel or bladder control. A tear in the dura mater, known as a dural tear, can cause spinal fluid to leak, which might require a second procedure to repair.
- Excessive Bleeding: Spine surgery involves working near major blood vessels. While surgeons take great care to control bleeding, unexpected blood loss can occur. In some cases, a blood transfusion may be necessary.
- Anesthesia Complications: As with any surgery requiring general anesthesia, there are risks of adverse reactions to the anesthetic drugs. These can range from nausea and confusion upon waking to more severe, though rare, complications like allergic reactions, heart attack, or stroke.
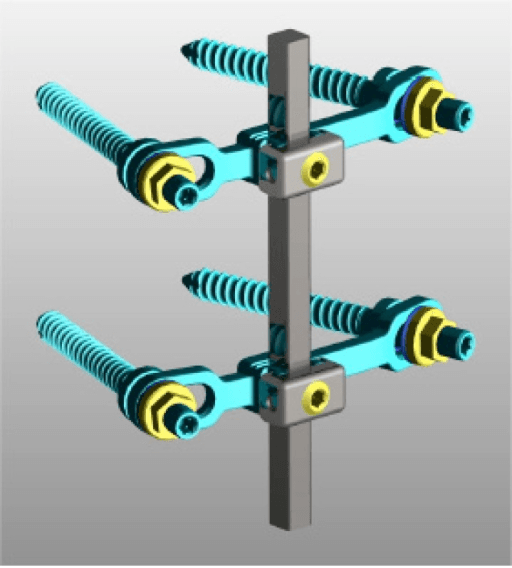
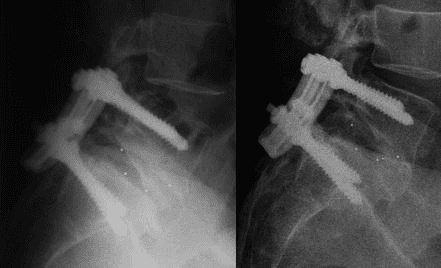
- Implant Misplacement: The screws, rods, and cages used to stabilize the spine must be placed with precision. If a screw is misplaced, it can irritate a nerve or fail to provide adequate support, potentially requiring another surgery to correct it.
The Long-Term Complications of PLIF Surgery
Even after a successful surgery and initial recovery, some issues can arise months or even years later.
- Failed Fusion and Pseudarthrosis: The primary goal of fusion surgery is for the vertebrae to grow together into a single, solid bone. If this fails to happen, a condition known as pseudarthrosis or non-union occurs. This is one of the most common long-term complications and a leading cause of persistent pain after surgery. Revision surgery is often needed to achieve a solid fusion.
- Adjacent Segment Disease (ASD): When one or more levels of the spine are fused, they no longer move. This transfers extra stress and strain to the spinal joints above and below the fused segment. Over time, this added stress can accelerate the degeneration of these adjacent discs and joints, leading to new pain, stenosis, or instability. This may eventually require another surgery at the adjacent levels.
- Persistent Pain or Symptoms: Unfortunately, PLIF surgery is not a guaranteed cure. Some patients may continue to experience back or leg pain even after a technically successful procedure with a solid fusion. This can be due to a variety of factors, including scar tissue formation around nerves (epidural fibrosis), permanent nerve damage from the original condition, or other underlying issues.
- Implant-Related Issues: Over the long term, the metal hardware can sometimes cause pain or irritation. While the implants are designed to be permanent, they may need to be removed in a later surgery if they are causing problems after the fusion is solid.
- Narcotics Addiction: The risk of opioid and narcotic addiction after PLIF surgery is a significant concern, as these medications are often prescribed to manage post-operative pain. While opioids can be effective for short-term pain relief, prolonged use or misuse can lead to dependency or addiction. A study found that approximately 8.4% of patients who underwent lumbar spine surgery, including fusion, were persistent opioid users two years after surgery. Another study reported that 15-18% of opioid-naïve patients developed chronic opioid use after standard spinal procedures.
Live Pain-Free Without Complications
If you’re seeking relief from lower back pain, have been recommended for PLIF surgery, or are still dealing with chronic neck pain after a failed fusion surgery, we can help improve your quality of life and enable you to live pain-free - without complications. Deuk Laser Disc Repair (DLDR) is the most advanced laser spine surgery in the world and is used as an alternative to dangerous surgeries like PLIF. We livestream our surgeries with our patient’s written consent, to provide complete transparency as to how Deuk Laser Disc Repair changes lives. Watch a livestream of a patient surgery who chose DLDR rather than the recommended PLIF by their former surgeon.
It takes less than an hour, and our patients leave the outpatient clinic a few hours after surgery without pain or the need for addictive painkillers. Our success rate is 99.5%, and we have treated thousands of patients who are now living pain-free.
Take The First Step Now
Upload your latest MRI for a free review and a personal consultation with acclaimed spinal surgeon Dr. Ara Deukmedjian, M.D., founder of Deuk Spine Institute and creator of the Deuk Laser Disc Repair® procedure. Our team will contact you to help you regain your life.
