What is Spinal Fusion Surgery?
Cervical spinal fusion is a surgical procedure that joins or “fuses” two or more vertebrae in the neck (the cervical spine) so they heal into one solid bone. Its primary purpose is to stabilize the spine, relieve pain, and address issues caused by damaged discs, joints, or abnormal movement. The C5-C6 and C6-C7 segments experience the most motion and stress in the cervical spine, making them more prone to cervical issues.
What are the most common areas affected in the cervical spine?
In the cervical spine (neck), there are seven vertebrae, labeled C1–C7, with discs between C2 and C7. Not all levels are equally prone to problems.
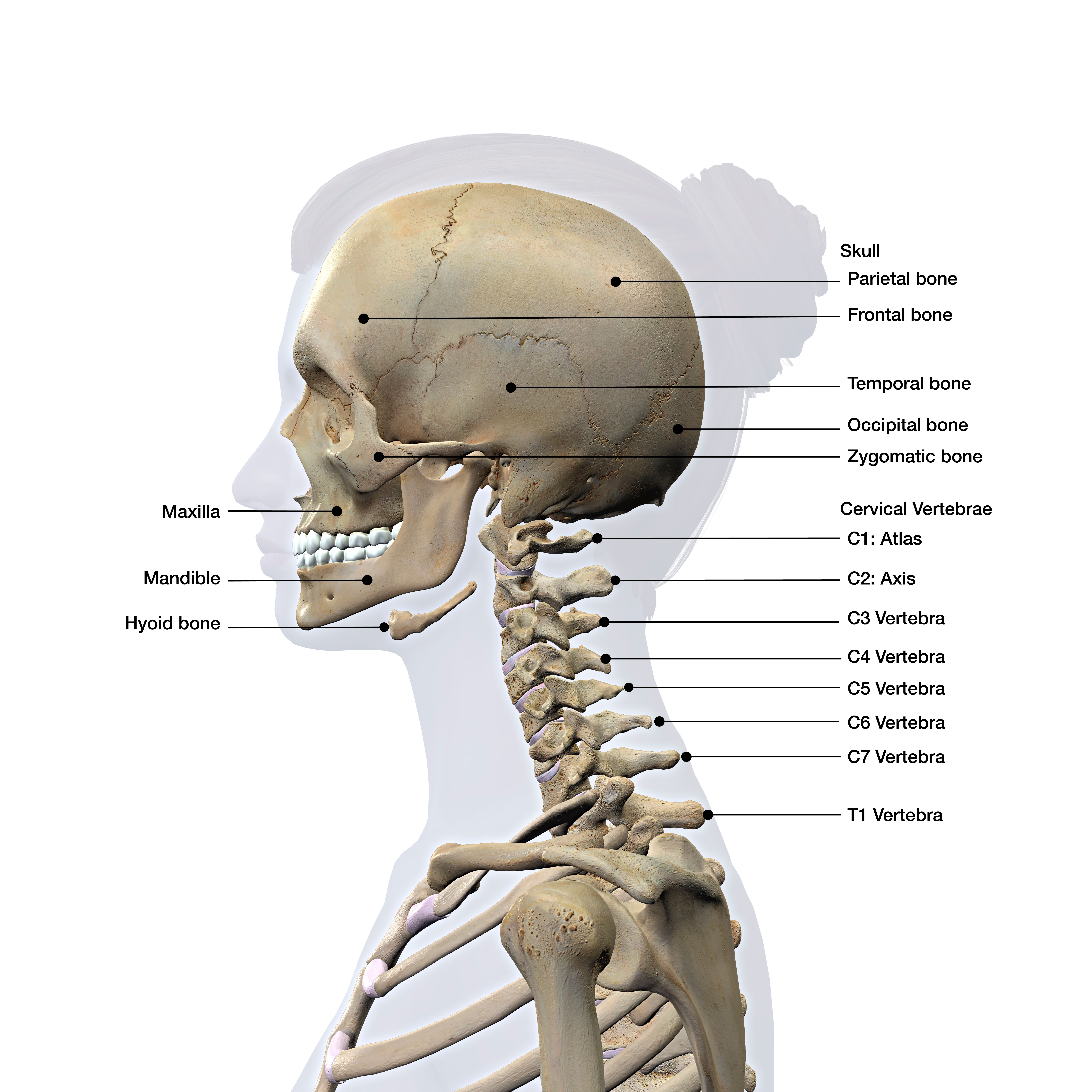
- The C5–C6 segment is the most common site for disc degeneration and herniation, leading to pain, numbness, or weakness that radiates into the biceps, wrist extensors, and possibly the thumb.
- The C6–C7 segment is the second most frequently affected level, with symptoms that can radiate into the triceps, forearm, and middle finger.
- The C4–C5 segment is less frequently affected; however, problems in this area can still influence the shoulder and deltoid muscles.
- The C3–C4 segment is the least affected, but when it is affected, it may cause neck pain, headaches, or weakness in the upper shoulders.
What conditions does cervical fusion surgery treat?
Cervical spinal fusion is needed when the spine becomes unstable, compressed, or severely degenerated, and when instability or nerve damage threatens function or quality of life. These conditions may include:
Degenerative Disc Disease (DDD)
The discs between vertebrae wear down with age or stress, leading to long-term neck pain, stiffness, and nerve irritation. Fusion stabilizes the segment and prevents additional motion-related pain.
Cervical Disc Herniation
A herniated (slipped or ruptured) disc can press on the spinal cord, causing neck pain, arm pain, numbness, tingling, or nerve root weakness. If symptoms persist or worsen, fusion is often combined with disc removal (anterior cervical discectomy and fusion, ACDF).
Cervical Spinal Stenosis and Myelopathy
Spinal stenosis is a narrowing of the spinal canal that compresses the spinal cord. Causing clumsiness in the hands, gait imbalance, weakness, or issues with bowel and bladder control. Fusion is often required together with decompression (laminectomy or discectomy) to prevent further spinal cord injury.
Spinal instability can result from trauma (like fractures and dislocations), arthritis, or surgery. When vertebrae move abnormally, fusion is performed to restore stability and prevent additional movement.
Cervical Fractures
Some unstable neck fractures, such as those caused by accidents or falls, require fusion to stabilize the spine. safeguard the spinal cord and promote healing.
Cervical Deformities
Cervical deformities include conditions like kyphosis (forward curvature) or scoliosis in the neck. Fusion helps realign the spine and prevents further progression.
Tumors or Infections
When cancer, bone tumors, or severe infections like osteomyelitis weaken the cervical spine, it can cause problems. Fusion stabilizes the area after removing diseased tissue.
What are the types of cervical spinal fusion procedures?
Traditional open spinal surgery involves a longer incision, usually 2-5 inches or more, to access the spine directly. The surgeon retracts (pulls back) the muscles and other soft tissues to get a clear and wide view of the surgical site. Open surgery is a well-established technique that is understood and reliable, but it has several disadvantages.
- More Tissue Damage: The extensive muscle retraction can cause significant damage to muscles, ligaments, and nerves, leading to increased postoperative pain.
- Longer Recovery: Due to the tissue damage, recovery is often more prolonged and more painful. Patients may require a more extended hospital stay.
- Greater Risk: The larger incision and more invasive nature can lead to a higher risk of blood loss, infection, and other complications.
- More Scarring: The longer incision results in a more noticeable scar.
Minimally Invasive Cervical Spinal Fusion (MISS) uses smaller incisions (often less than an inch) and specialized tools, such as tubular retractors and endoscopes, to access the spine. Instead of cutting and pulling back muscles, the surgeon works between the muscle fibers. There are several advantages of MISS over open surgery:
- Less Tissue Damage: By working between muscle fibers, MISS avoids the extensive muscle dissection associated with open surgery, resulting in less post-operative pain and a faster recovery.
- Smaller Incisions: Results in less scarring and reduced blood loss.
- Shorter Hospital Stay: Many patients can be discharged from the hospital within a day or two, and some procedures can even be done on an outpatient basis.
- Reduced Risk of Complications: Less blood loss and reduced tissue damage may lead to a lower risk of infection.
- Less Versatility: MISS may not be suitable for complex cases, severe spinal deformities, or revision surgeries.
How does open disc surgery differ from minimally invasive disc surgery?
Cervical spinal fusion can be performed using various surgical approaches and techniques, depending on the patient’s condition, the problem’s location, and the surgeon’s preference. Here are the main types
Anterior Cervical Discectomy and Fusion (ACDF)
ACDF is a common procedure that approaches the neck from the front (anterior). The surgeon removes the damaged disc, relieves pressure on the nerve or spinal cord, then inserts a bone graft or spacer between the vertebrae and secures it with a plate and screws. This procedure treats herniated discs, degenerative disc disease, and spinal stenosis at one or two levels.
Anterior Cervical Corpectomy and Fusion (ACCF) ACCF is also performed from the front of the neck, but instead of just removing the disc, the surgeon removes part (or all) of a vertebral body, plus adjacent discs, to relieve wider spinal cord compression. A larger bone graft or cage is placed, and then it is secured in position with hardware. This procedure treats multi-level stenosis, bone spurs, tumors, or trauma.
Posterior Cervical Disc Fusion (PCDF)Post cervical fusion approaches the neck from the back (posterior), placing bone grafts along the back of the spine and securing them with screws and rods for stability. The procedure is most often used to treat multi-level instability, fractures, deformities (such as kyphosis or scoliosis), or when anterior surgery is not possible.
Posterior Cervical Laminectomy/Laminoplasty with Fusion Also approaching the neck from the back, the surgeon removes or reshapes the lamina (the roof of the vertebra) to decompress the spinal cord. A fusion is performed simultaneously to stabilize the spine. This procedure is best suited for cervical myelopathy (cord compression) and multi-level stenosis.
Combined Anterior and Posterior Fusion Some severe cases that may present with high instability, complex deformity, tumors, or trauma require both front and back approaches in the same surgery. This approach provides the highest stability but is also the most extensive procedure.
Minimally Invasive Cervical Fusion Minimally invasive cervical fusion uses smaller incisions and specialized instruments for less muscle disruption and quicker recovery.
A study forecasting trends from 2020 to 2040 predicts increases. in surgical volume for anterior cervical discectomy and fusion (ACDF) and posterior cervical decompression and fusion (PCDF), reflecting an aging population
How does open disc surgery differ from minimally invasive disc surgery?
Traditional open spinal surgery involves a longer incision, usually 2-5 inches or more, to access the spine directly. The surgeon retracts (pulls back) the muscles and other soft tissues to get a clear and wide view of the surgical site. Open surgery is a well-established technique that is understood and reliable, but it has several disadvantages.
- More Tissue Damage: The extensive muscle retraction can cause significant damage to muscles, ligaments, and nerves, leading to increased postoperative pain.
- Longer Recovery: Due to the tissue damage, recovery is often more prolonged and more painful. Patients may require a more extended hospital stay.
- Greater Risk: The larger incision and more invasive nature can lead to a higher risk of blood loss, infection, and other complications.
- More Scarring: The longer incision results in a more noticeable scar.
The Deuk Difference
Unlike invasive cervical spinal surgeries, the Deuk Spine Institute performs the least invasive cervical procedure in the world—the proprietary Deuk Laser Disc Repair (DLDR). DLDR is done without cutting or harming healthy muscle, fascia, or bone, without using risky hardware and without post-operative pain. Best of all, recovery time is less than three days.
How we do it
An endoscope is inserted through a small skin incision at the affected level, and a laser removes damaged tissue from the annular tear at the back of the disc, eliminating the source of pain. In some cases where facet arthritis is also a concern, we use our proprietary Deuk Plasma Rhizotomy to relieve arthritic joint pain.
Watch the surgery
Our goal is to be completely transparent about our process and procedures for treating back issues, helping our patients and others suffering from severe back and neck pain return to fully living their lives. We livestream our surgeries with our patients' written consent, giving you the chance to see our technique firsthand.
What to expect
It takes less than an hour, and our patients leave our outpatient clinic a few hours after surgery feeling no pain and without needing addictive painkillers. They come back to our clinic the next day for a postoperative checkup.
Our success rate
Our success rate is 99.5%, and we have treated thousands of patients who are now living. pain-free. It took 20 years and thousands of surgical hours to discover the root cause of chronic back pain and the effectiveness of lasers in treating it.
Our commitment
We understand how damaging chronic back pain can be to your life. As neurosurgeons and healthcare providers, we are dedicated to eliminating and curing back pain once and for all. Your back is one of the most vital parts of your body, composed of a complex network of nerves, bones, and tissues. That’s why our entire team is committed to providing the highest quality patient care. We hold each other accountable and uphold high standards for every team member.
Make the first move to a pain-free life
If you’re seeking back pain relief, have been recommended for a spinal fusion, or are still coping with chronic back pain after a failed fusion surgery, we can help enhance your quality of life and guide you toward a pain-free future.
Upload your latest MRI for a free review and a personal consultation with Dr. Ara Deukmedjian, M.D., founder of Deuk Spine Institute, who developed the Deuk Laser Disc Repair® procedure. Our team will contact you to help you regain control of your life.