If you're dealing with severe back or neck pain, your surgeon will most likely recommend spinal fusion surgery. With over 1.5 million procedures expected by the end of 2025, it’s a common treatment path. However, it's a highly invasive, major operation with significant implications that deserve careful consideration.
This article will walk you through the common myths and realities of spinal fusion surgery. Our goal is to provide a clear, balanced view to help you understand what to expect if you're considering a fusion.
MYTH 1: You'll Recover in Just a Few Months
REALITY: Full recovery often takes 6 months to a year, or even longer.
While surgeons may suggest a quick turnaround, the healing process for spinal fusion is extensive. Even healthy patients typically require a significant amount of time to get back to their normal lives.
What to Consider:
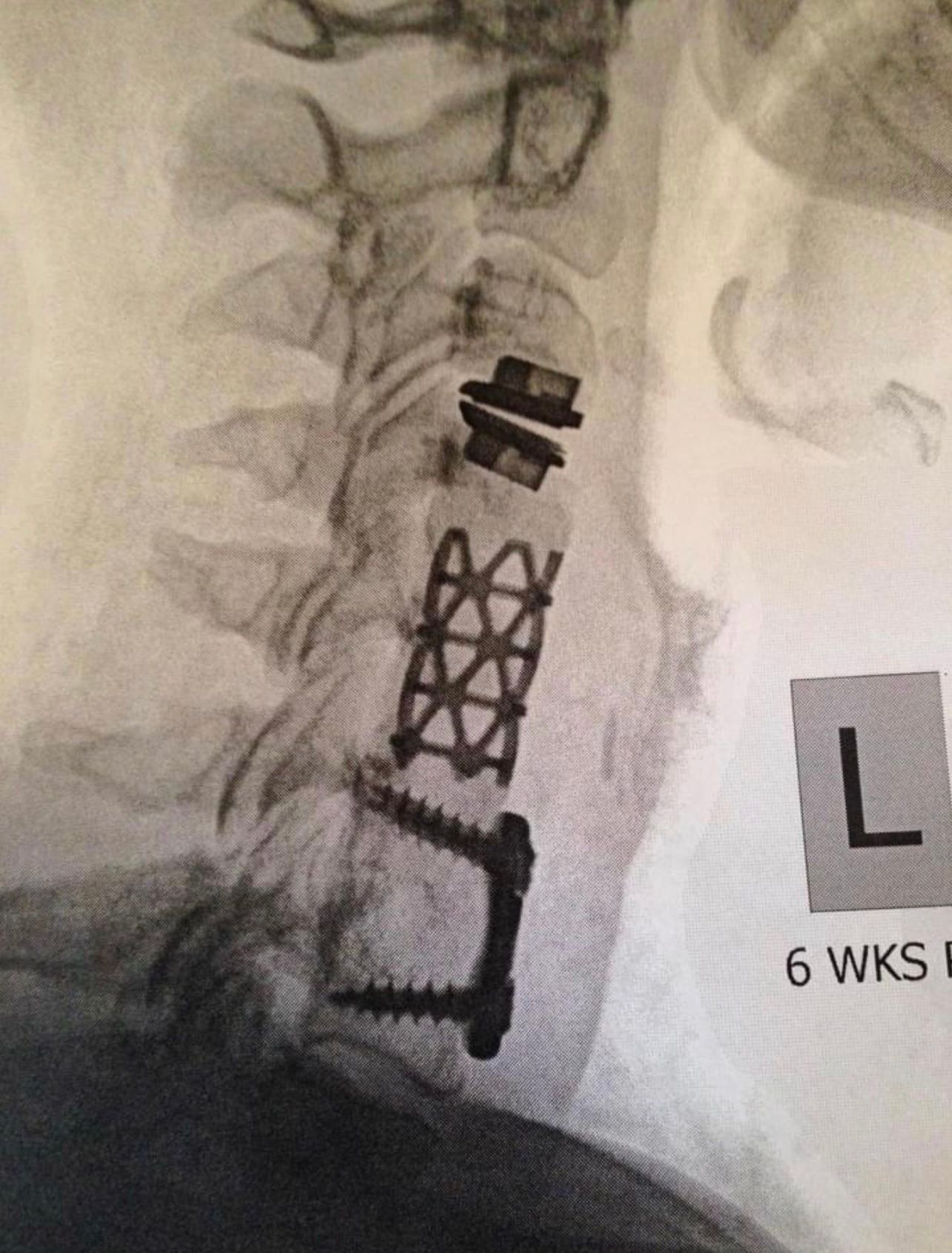
- Extensive Healing: The surgery involves cutting through muscle and drilling into bone to place metal hardware like screws and rods. Your body needs a long time to heal from this trauma, often taking at least six months.
- Post-Hospital Care: Many patients are not ready to go straight home from the hospital. They may need to spend time in a rehabilitation or convalescent center for ongoing care and physical therapy until they are strong enough to manage at home.

- Ongoing Treatments: Recovery isn't just about resting. It involves a structured regimen that can include physical therapy, occupational therapy to relearn daily tasks, pain management appointments, and other treatment modalities, all of which extend the recovery timeline
Myth 2: The Surgery Guarantees Permanent Pain Relief
REALITY: Up to 40% of patients experience persistent pain after surgery.
Spinal fusion does not always resolve the underlying pain. A significant number of patients continue to have chronic pain, a condition sometimes called Failed Back Surgery Syndrome (FBSS).
What to Consider:
- The Bones Don't Fuse: Sometimes, the vertebrae fail to fuse together properly. This condition, known as pseudoarthrosis, can be a source of continued pain and instability.
- Hardware Complications: The metal implants used in the surgery can fail. Screws may loosen or break, and rods can slip out of place, sometimes impacting nearby nerves and tissues.
- Adjacent Segment Disease: The fusion creates a rigid section in your spine, which increases stress on the vertebrae above and below it. This can accelerate degeneration in those adjacent discs, leading to new sources of pain.
- Post-Operative Pain: The surgery itself is a major source of pain that requires careful management, often with strong pain medications like narcotics, especially in the initial recovery period.
MYTH 3: Minimally Invasive Surgery Is Always Safer
REALITY: Minimally invasive techniques have similar long-term risks.
Minimally Invasive Spine Surgery (MISS) uses a smaller incision, which can reduce muscle damage and scarring. However, the fundamental procedure of fusing vertebrae remains the same, along with its associated long-term complications.
What to Consider:
- Internal Hardware: Cages, rods, and screws are still placed into the spine to create the fusion. This carries the same risks of hardware failure and damage to adjacent bone, regardless of the incision size.
- Requires High Precision: Working through a smaller opening gives the surgeon a limited view of the spine. This demands exceptional skill and precision to place hardware correctly and avoid damaging delicate nerves.

- Significant Pain: While the incision is smaller, the internal work on the bone and discs is just as intensive. Pain levels after MISS can be comparable to traditional open surgery and often require narcotic painkillers for management.
MYTH 4: All Spine Surgeons Are the Same
REALITY: The surgeon's training and specialty can make a big difference.
There are important distinctions between neurosurgeons and orthopedic surgeons who specialize in spine surgery. Their training backgrounds influence their surgical approaches and areas of expertise.
What to Consider:
- Neurosurgeons: This specialty focuses on the nervous system, including the spinal cord and its complex network of nerves. Neurosurgeons are extensively trained in the delicate techniques needed to operate safely around these structures, which is critical for procedures that approach the spine from the back (posterior) PLIF or side (lateral) XLIF.

- Orthopedic Surgeons: This specialty focuses on the musculoskeletal system, including bones and joints. Spine-focused orthopedic surgeons are experts on the spine's structure. Some may be more accustomed to an anterior approach, ALIF, which accesses the spine from the front and involves less direct manipulation of the spinal nerves. However this approach requires a large incision through the stomach and comes with serious risks and complications.
The Better Way: Deuk Laser Disc Repair (DLDR)
The Better Way: Deuk Laser Disc Repair (DLDR)
For patients suffering from debilitating pain or severe instability, the benefits of spinal surgery might seem to outweigh the risks significantly. However, as you can see, they are not procedures without consequences. There is one procedure that has none of these consequences. My revolutionary procedure, Deuk Laser Disc Repair (DLDR),

offers a safer way to alleviate neck or back pain without risk of collateral damage, as it avoids the muscles, nerves, ligaments, tendons, and joints.
A Game-changing Procedure
DLDR is a minimally invasive form of endoscopic spine surgery performed in a modern surgery center under sedation, allowing patients to relax during the procedure. The procedure is done endoscopically using a high-definition camera inserted through a tiny 4mm incision to view the injured area. DLDR uses a precision laser to vaporize the herniated tissue. Fascia, muscles, ligaments, or bone are not damaged or removed. Fusions and artificial discs are not necessary. After surgery, patients wake up to immediate relief and a surgical scar so small that the surgeon can cover it with a Band-Aid.
Watch Deuk Laser Disc Repair in Action
Our goal is to be completely transparent about our process and procedures for treating back issues. We livestream surgeries with our patients’ written consent, allowing you to observe our technique.
Make the First Move to Move Pain-Free
Upload your latest MRI for a complimentary review and consultation with me, Dr. Ara Deukmedjian, M.D., founder of Deuk Spine Institute and creator of the procedure. Our team will reach out to you to help you regain your life.
