INTRODUCTION
Lumbar spinal fusion is a surgical procedure that joins two or more vertebrae in the lower back (lumbar spine) to create a single, solid bone. This is typically done to stabilize the spine and alleviate pain caused by several conditions. The specific discs and vertebrae most likely to be affected and require fusion are those in the lower half of the lumbar spine, particularly the L4-L5 and L5-S1 segments
WHY ARE THESE DISCS OFTEN THE CULPRITS?
The L4-L5 segment is the most common level for lumbar spinal fusion because it is a major weight-bearing and motion-producing area of the spine, making it highly susceptible to degenerative changes and injuries.
The L5-S1 segment, the second most common level for fusion. because the segment connects the lumbar spine to the sacrum, and like L4-L5, it experiences significant stress and is prone to conditions like degenerative disc disease and spondylolisthesis (a condition where a vertebra slips out of place).
WHAT CONDITIONS NECESSITATE LOWER BACK SURGERY?
The most common conditions that may require lumbar spinal fusion, include:
- Degenerative Disc Disease (DDD): This is the most common reason for lumbar fusion. The discs between the vertebrae wear down over time, leading to pain and instability. The L4-L5 and L5-S1 discs are under the most stress from body weight and movement, making them highly susceptible to degeneration.
- Spondylolisthesis: This condition occurs when one vertebra slips forward over the one below it. It is often caused by a defect in the pars interarticularis, a small segment of bone in the vertebra. The L5 vertebra slipping over the S1 is a very common scenario, and fusion is often required to correct the alignment and stabilize the spine.
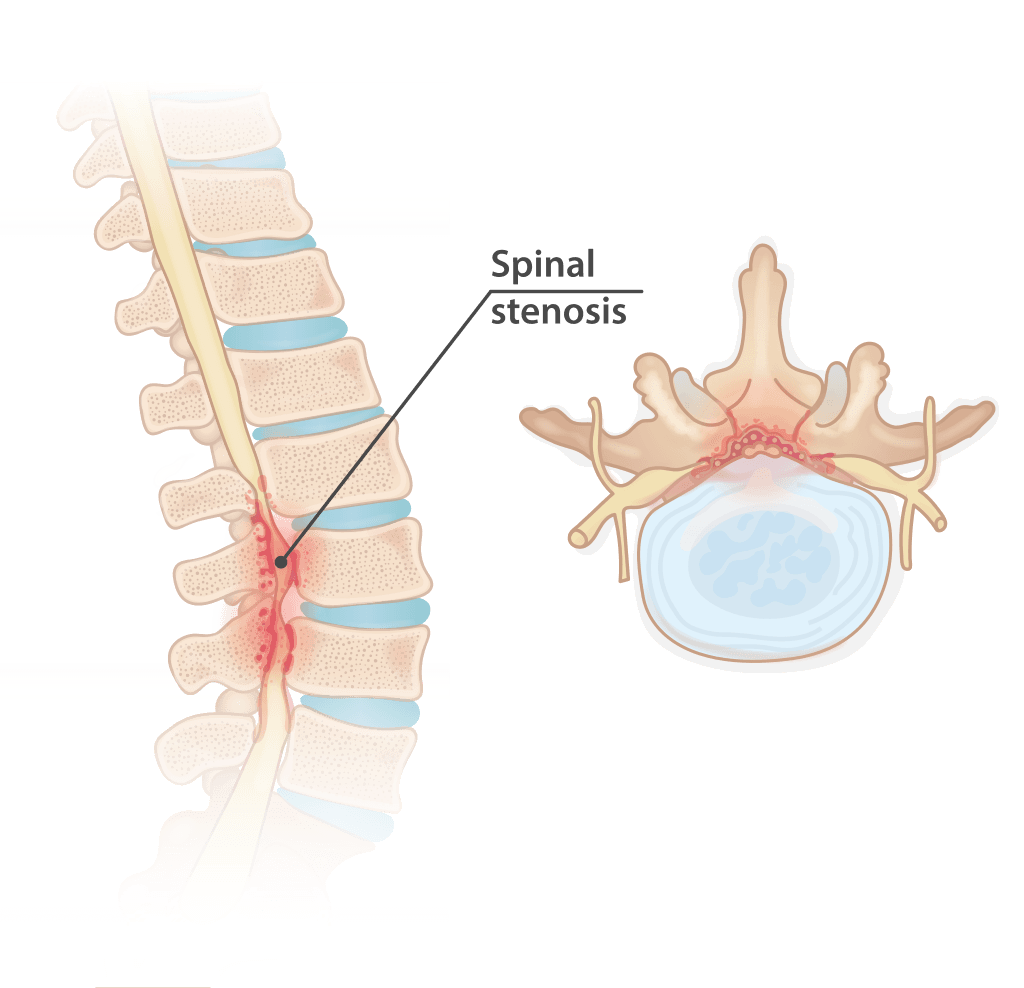
- Spinal Stenosis: This is a narrowing of the spinal canal, which can put pressure on the spinal nerves. While sometimes treated with decompression alone, fusion may be necessary to maintain stability after the bone and tissue causing the narrowing are removed.
- Herniated Disc: In severe or recurrent cases, or when a previous surgery (such as a discectomy) has caused spinal instability, a fusion may be performed to stabilize the affected segment and prevent further herniation.
- Spinal Deformities: Conditions like scoliosis (sideways curvature) or kyphosis (forward curvature) may require a multi-level fusion to correct the abnormal curve and provide stability.
- Spinal Fractures, Tumors, or Infections: Fusion is often used to stabilize the spine after a vertebral fracture or to provide support after the removal of a tumor or treatment of an infection.
TYPES OF LUMBAR INTERBODY FUSION (LIF) PROCEDURES
The most common types of lumbar interbody fusion (LIF) procedures are named based on the surgical approach and the specific technique used to fuse the vertebrae.
These procedures involve removing the intervertebral disc and replacing it with a bone graft and/or an implant to fuse the two vertebrae. They are distinguished by the direction the surgeon approaches the spine.
- Anterior Lumbar Interbody Fusion (ALIF): The surgeon accesses the spine from the front (anterior) through an incision in the abdomen. This approach is often used to treat conditions like degenerative disc disease and spondylolisthesis.
- Posterior Lumbar Interbody Fusion (PLIF): The surgeon accesses the spine from the back (posterior). This procedure involves removing the disc and inserting a bone graft and an implant from the rear. Screws and rods are often used to provide additional stability.
- Transforaminal Lumbar Interbody Fusion (TLIF): Similar to PLIF, this procedure is also performed from the back. However, the surgeon accesses the spine from a more lateral (side) position through the foramen (the natural opening where a nerve root exits the spinal canal). This approach is designed to minimize nerve root manipulation and potential damage.
- Lateral Lumbar Interbody Fusion (LLIF): Also known as Extreme Lateral Interbody Fusion (XLIF) or Direct Lateral Interbody Fusion (DLIF), this procedure is performed with the patient on their side. The surgeon accesses the spine through a small incision on the side of the body, passing through or around the psoas muscle. This is often a minimally invasive technique.
- Oblique Lumbar Interbody Fusion (OLIF): This is a variation of the lateral approach where the surgeon enters the spine from an oblique angle, sparing the psoas muscle.
All spinal fusion procedures require a bone graft, which acts as a scaffold for new bone growth to fuse the vertebrae. The types of bone grafts include:
- Autograft: Bone harvested from the patient's own body, usually from the hip (iliac crest).
- Allograft: Bone from a donor, typically a cadaver.
- Synthetic Grafts: Man-made materials like ceramics, calcium, and phosphate compounds.
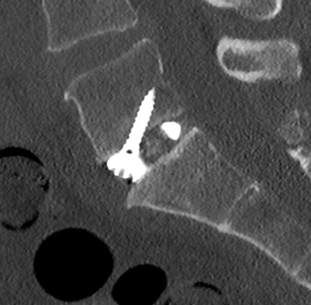
In many cases, surgical instrumentation such as metal plates, screws, and rods is also used to hold the vertebrae in place while the fusion process occurs. This provides immediate stability and improves the chances of a successful fusion.
MINIMALLY INVASIVE SPINAL SURGERY (MISS)
Many of the procedures listed above can be performed using either traditional open surgery or a minimally invasive technique.
- Open spinal surgery involves a larger incision and more extensive muscle dissection to expose the spine.
- Minimally invasive spinal surgery (MIS) uses smaller incisions and specialized instruments to perform the surgery with less tissue damage, potentially leading to less blood loss, a shorter hospital stay, and a faster recovery.
In short, you can have a:
- Lumbar Spinal Fusion (open or minimally invasive)
- Endoscopic Lumbar Spinal Fusion (a type of minimally invasive fusion)
- Laser Spine Surgery (a type of minimally invasive decompression, not fusion)
WHAT IS THE DIFFERENCE BETWEEN SPINAL FUSION SURGERY AND SPINAL DECOMPRESSION SURGERY?
It is critical to differentiate minimally invasive spinal fusion and minimally invasive decompression. Minimally invasive spinal fusion and minimally invasive spinal decompression are two distinct types of surgical procedures, although both are performed on the spine using smaller incisions and specialized instruments. The key difference lies in their surgical goal.
- Minimally Invasive Spinal Fusion: The primary goal of a minimally invasive spinal fusion is to stabilize the spine. It permanently joins two or more vertebrae to stop painful motion. The goal is to permanently connect two or more vertebrae into a single, solid bone to treat conditions that involve instability or painful motion, like:
- Degenerative Disc Disease: Where a worn-out disc causes instability and pain.
- Spondylolisthesis: When one vertebra slips forward on another.
- Spinal Fractures or Deformities: Where the spine needs to be stabilized after a break or to correct a curve.
This is a more complex procedure. In addition to accessing the spine through small incisions, the surgeon must remove the intervertebral disc and insert a bone graft or a synthetic cage into the space. Metal hardware like screws and rods are then used to hold the vertebrae in a fixed position while the bone graft fuses the bones together over time.
This results in a permanent loss of motion at the fused level.
- Minimally Invasive Decompression: The primary goal of a minimally invasive decompression is to relieve pressure on spinal nerves. It is a "de-roofing" procedure that removes a source of compression, but it does not stabilize the spine or fuse vertebrae together. The goal is to create more space in the spinal canal around a nerve root where bone, disc, or soft tissue is pressing on a nerve, causing pain, numbness, or weakness in the legs or arms. Common conditions include:
- Spinal Stenosis: A narrowing of the spinal canal.
- Herniated Disc: When the soft center of a disc pushes out and irritates a nerve.
The surgeon uses a small incision and a tubular retractor to access the spine. Through this small tunnel, they use small instruments to remove the specific source of compression, such as a portion of a herniated disc (a discectomy) or overgrown bone and ligaments (a laminectomy or foraminotomy). The goal is to alleviate the nerve-related symptoms by removing the obstruction. The spine remains mobile, as no fusion takes place.
THE DEUK DIFFERENCE
Unlike invasive lumbar spinal surgeries, the Deuk Spine Institute performs the most minimally invasive spinal procedure in the world–the proprietary Deuk Laser Disc Repair, performed without cutting or compromising healthy muscle, fascia, or bone, without the use of risky hardware, and without post-operative pain. Best of all, the recovery time is less than three days.
HOW IT’S DONE
We utilize our proprietary Deuk Laser Disc Repair procedure, a patented, minimally invasive endoscopic laser spine surgery - and the only one of its kind in the world - to treat back and neck pain. An endoscope is inserted through a small opening in the skin at the affected level, and a laser is used to remove damaged tissue from the annular tear at the back of the disc, thereby eliminating the source of pain. In certain patient cases where facet arthritis is also a concern, we utilize our proprietary Deuk Plasma Rhizotomy to alleviate arthritic joint pain.
SEE THE SURGERY LIVE
Our goal is to provide complete transparency into our process and procedures for curing back issues, helping our patients and others suffering from debilitating back and neck pain return to living their lives fully. We livestream our surgeries with our patients' written consent, allowing you to witness our technique.
WHAT TO EXPECT
It takes less than an hour, and our patients walk out of our outpatient clinic a few hours post op with no pain and no need for addictive painkillers. They come back to our clinic the next day for a post operative follow-up.
OUR SUCCESS RATE
Our success rate is 99.5% and we have treated thousands of patients who are now living pain-free. It took 20 years and thousands of surgical hours to discover the root cause of chronic back pain and the effectiveness of lasers in treating it.
WE’RE HERE TO HELP
We know how destructive chronic back pain can be to your life. As neurosurgeons and healthcare professionals, we have dedicated ourselves to eliminating and curing back pain once and for all. If you’re looking for back pain relief, if you’ve been recommended for a spinal fusion, or are continuing to live with chronic back pain after failed fusion surgery, we can get your quality of life back and help you live pain-free.
OUR COMMITMENT
Your back is one of the most vital components of your body, comprising a complex network of nerves, bones, and tissues. It’s why our entire staff is uncompromising in our commitment to providing the highest levels of patient care. We hold each other accountable and set high expectations for every member of our team.
TAKE THE FIRST STEP TO A PAIN-FREE LIFE
Upload your most recent MRI to receive a free review and consultation with Dr. Ara Deukmedjian, M.D., the founder of Deuk Spine Institute, who developed the Deuk Laser Disc Repair® procedure. Members of our team will reach out to help you regain control of your life.
