Introduction
Back pain affects every aspect of your life. When conservative treatments fail, many patients are told that spinal fusion is their only option. This highly invasive, major surgery involves permanently connecting two or more vertebrae in your spine to eliminate motion between them. It has numerous surgical risks and many long-term complications.
Advances in medical technology and a deeper understanding of spinal mechanics have led to several procedures that can be performed instead of a fusion, some of which are more effective than others, but in the end, none of them, including fusion, cures back pain. In this article, we will explore some of the more predominant standard options and the one innovative alternative that addresses back and neck pain at its source and cures it, forever.
Four Common Standard Options
1. Artificial Disc Replacement
Artificial disc replacement (ADR) is a surgical procedure where a damaged or degenerated spinal disc is removed and replaced with a prosthetic, artificial disc. Unlike fusion, which eliminates movement, ADR is designed to preserve the natural motion of the spine at the affected spinal level. It’s commonly performed in the cervical (neck) or lumbar (lower back) spine for patients with degenerative disc disease, disc herniation, or discogenic pain.
Complications: As with any surgery, risks include infection, bleeding, and nerve damage. Because the disc is an implant, there are several complications specific to the implanted artificial disc:
- Subsidence: the implant sinks into the bone if the vertebrae are weak.
- Wear and tear: Long-term exposure to particle debris may cause inflammation.
- Heterotopic ossification (HO): unwanted bone forms around the implant, gradually limiting motion and mobility.
- Loss of motion: despite ADR’s purpose, scar tissue or HO can make the level act like a fusion.
- Nerve damage: Nerve root irritation or injury that causes weakness, numbness, or tingling.
- Vascular or Organ Complications: Post-surgical damage to nearby blood vessels or organs may cause delayed bleeding, bowel/bladder issues, or retrograde ejaculation in men (from injury to sympathetic nerves).
Why It Might Not Work: ADR mainly targets pain caused by a specific damaged disc. It does not fix problems related to spinal joints (facet joints) or widespread arthritis. If pain originates from multiple sources, simply replacing one disc may not provide complete relief. ADR typically reduces stress on nearby discs compared to fusion; however, adjacent segment degeneration can still occur over time.
Some patients continue to experience pain even after a technically “successful” surgery. In one study, the overall clinical failure rate was 26% at a 2-year follow-up. Causes of failure included facet pathology in 50% of failure cases, implant complications in 5% of all patients, and 21% of failure cases. If ADR fails, revision surgery usually involves removing the implant and switching to spinal fusion.
2. Spinal Cord Stimulators
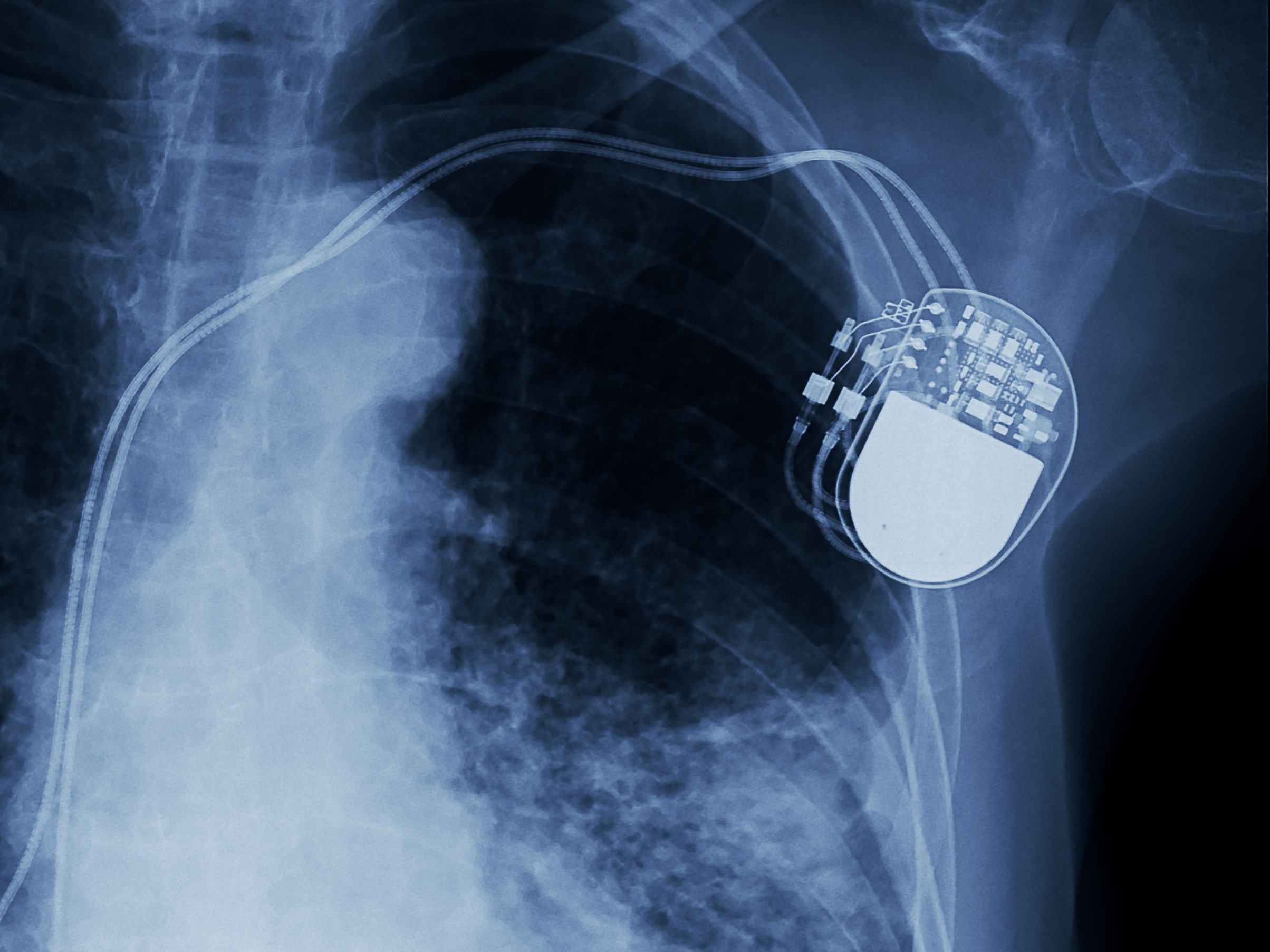
A spinal cord stimulator (SCS) is a device, similar to a pacemaker, that is surgically implanted under the skin. It delivers low levels of electrical pulses directly to the spinal cord to block pain signals before they reach the brain. Mechanically, the leads that deliver the electrical pulses can move or break, requiring revision surgery. Additionally, the battery may wear out. But there are there are more than mechanical complications.
Complications: Because placing a SCS is invasive surgery, the surgical risks are typically caused by the surgeon:
- Excessive and unnecessary bleeding during and after surgery from muscle trauma.
- Infection, including meningitis, epidural abscess, osteomyelitis, or discitis.
- Destruction of normal muscle, stabilizing bones including the lamina (laminectomy) and spinous process, and ligaments such as the supraspinous, interspinous, and ligamentum flavum.
- Excessive scar tissue forms around the spinal cord and nerves after placement surgery.
Why It Might Not Work: An SCS doesn't fix the underlying structural problem causing the pain; it only interrupts the pain signals. It's a form of pain management, not a cure. If the root cause of the pain, such as a herniated disc pressing on a nerve, worsens over time, the SCS may become less effective:
- Tolerance or adaptation – The nervous system may adapt to stimulation, decreasing its effectiveness.
- Changes in pain pattern – Pain might shift location or change in type, making the SCS less effective.
- Masking new problems – An SCS might hide the perception of a new spinal condition, delaying diagnosis.
A recent study indicates that reasons for SCS removal include issues related to efficacy. And inadequate pain relief (38%), followed by lead failure (15%) and infection (14%). Additional surgery may be necessary in over 90% of patients having SCS placement surgery.
3. Ultrasonic Spine Surgery
Ultrasonic spine surgery utilizes an ultrasonic bone scalpel that emits high-frequency sound waves to precisely cut through hard bone without damaging nearby soft tissues, such as nerves and blood vessels. This technique allows surgeons to decompress nerves with more accuracy and minimal collateral damage compared to traditional drills and burs.
Complications: Although designed to be safer for soft tissues, it remains a surgical procedure with risks including infection, bleeding, nerve damage, dural tears (a tear in the membrane covering the spinal cord), and nerve irritation. Because it acts like a jackhammer to the bone, the ultrasonic bone scalpel poses a risk for injury:
- Thermal Injury: Although ultrasonic tools are designed to minimize heat damage, improper use or technique can still harm surrounding nerves and tissues.
- Increased Pain: Occasionally, the destruction of bone or muscle during surgery can result in severe pain afterward.
- Bone instability or necrosis: Removing normal bone can lead to spinal instability, bone death (necrosis), and a higher likelihood of future surgery.
Postoperative surgical complications can also worsen pain:
- Adjacent segment disease (ASD): A spinal fusion can put extra stress on the vertebrae next to the fused segment. This can speed up degeneration and lead to new pain in those areas.
- Recurrent disc herniation: Another disc herniation might happen at the surgical site or at a neighboring level.
- Scar tissue formation: Postoperative scarring, known as epidural fibrosis, can develop around the nerves and cause chronic pain.
- Worsening pain: For some patients, back pain can become worse after the surgery instead of improving.
Why It Might Not Work: Ultrasonic surgery is a tool used for decompression, which involves removing bone or tissue that is pressing on nerves. It does not address spinal instability. If the spine is unstable, simply removing bone could worsen the problem. It is effective for specific tasks but does not resolve every spinal issue. The issues that may lead to failure of ultrasonic spine surgery include:
- Incorrectly Identifying the Pain Source: Back surgery might not succeed if the actual cause of pain, like a herniated or degenerated disc, is not correctly identified beforehand.
- Incomplete Nerve Decompression: Surgery may fail if it doesn’t fully relieve pressure on the pinched nerve root.
- Hardware Failure: During fusion procedures, devices such as screws, plates, or rods can break or loosen, leading to instability and pain.
- Failed Fusion (Pseudoarthrosis): If the vertebrae do not fuse properly, it can lead to ongoing instability and pain.
- Surgical Error: Incorrect screw placement or operating at the wrong spinal level are technical errors that can lead to ongoing or new pain.
The fact that studies of ultrasonic techniques generally report “no difference in symptom improvement” suggests that the failure (non-response) rate with ultrasonic methods is likely similar to conventional surgery in many settings. Although it’s less invasive, its success rate is identical to that of traditional spinal fusion surgery.
4. Epidural Steroid Injections
An epidural steroid injection (ESI) is a standard non-surgical treatment in which a powerful anti-inflammatory medicine, a corticosteroid, is injected into the epidural space around the spinal cord and nerve roots. The aim is to reduce inflammation and alleviate pain caused by conditions such as herniated discs, spinal stenosis, or sciatica.
Complications: Minimal surgical risks of ESI include pain at the injection site, spinal headache, insomnia or anxiety related to steroid effects, and elevated blood sugar. Repeated steroid injections can weaken nearby bones and tissues. More serious ESI complications include:
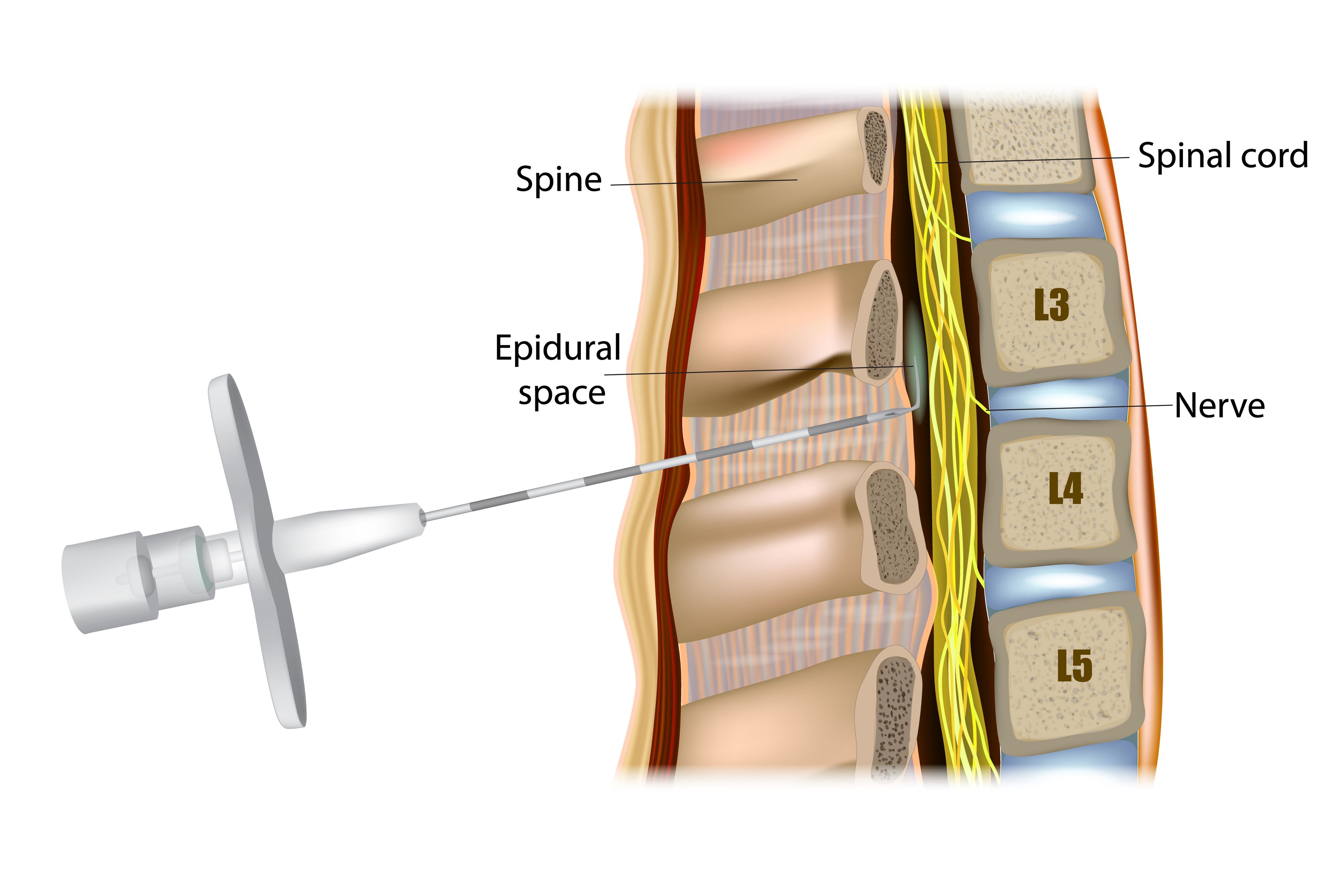
- Infection – superficial (skin) or deep (epidural abscess, meningitis)
- Bleeding/Hematoma – especially in patients on blood thinners
- Nerve Irritation or Damage – from needle trauma or pressure
- Arachnoiditis – rare inflammation of spinal nerves that can cause chronic pain
- Cushingoid effects (with repeated injections) – weight gain, facial puffiness, mood swings
- Stroke or Spinal Cord Infarction – if injected into an artery (extremely rare but catastrophic)
- Loss of bowel or bladder control – if nerves are severely affected
Why It Might Not Work: The relief from epidural injections is often temporary, lasting anywhere from a few weeks to several months. Here’s why they may not work:
- Wrong Pain Source: Steroids primarily reduce inflammation but do not address the underlying mechanical problem. If pain comes from structural issues, such as a large, herniated disc compressing nerves, severe spinal stenosis, or instability, steroids may have limited effectiveness.
- Wrong Pain Generator: Back and leg pain can originate from various sources (disc, facet joints, sacroiliac joints, muscles). If the injection targets the wrong level or structure, it may not provide any benefit.
- Nerve Damage Already Occurred: If nerves are significantly damaged, reducing inflammation won’t reverse the existing injury. Relief depends on whether the pain is due to irritation (which is reversible) or permanent damage (which is not).
The Innovative Alternative that Cures Back and Neck Pain
Deuk Laser Disc Repair (DLDR) is the most advanced laser spine surgery in the world. It is considered the best alternative to dangerous invasive surgeries like spinal fusion and artificial disc replacement. The surgeon uses an endoscope (a thin tube with a camera) to visualize the damaged disc and a precision laser to vaporize the herniated tissue that is pressing on nerves. It is the least invasive form of endoscopic spine surgery and does not compromise or weaken the health and integrity of the spine.

Complications: ZERO. In nearly 20 years of performing this surgery on more than 2,700 patients, there have been no complications because:
- Once the laser has removed the inflamed, painful section of the annular tear and the herniated nucleus pulposus, the endoscope is withdrawn, leaving an incision less than one-quarter inch that can be closed with a single stitch and a Band-Aid.
- This procedure is done without removing bone, using no implants or hardware, and it preserves the natural disc structure.
- The entire DLDR surgery typically takes about one hour, and the patient spends approximately 45 to 60 minutes in recovery before being discharged home. As an outpatient procedure, hospitalization isn't required, which reduces the risks linked to hospital-based surgery.
- Because the procedure does not cause the internal trauma of fusions or ADR, there is no postoperative pain, so opioids or powerful narcotic painkillers are not needed.
Why It Might Not Work: The procedure will only be effective if performed by a highly skilled surgeon with extensive experience in endoscopic laser techniques. A thorough diagnosis is essential to confirm if the pain is truly discogenic. It is not intended for conditions caused by cancer or infections.
DLDR is only performed at the Deuk Laser Institute by myself, Dr. Ara Deukmedjian, M.D. Over nearly 20 years, in over 2,700 surgeries performed, DLDR has eliminated, on average, 99.6% of discogenic pain.
Earning Your Trust
Choosing the proper treatment for your back or neck pain depends on an accurate diagnosis, but the decision must be based on trust, and that’s earned through the honesty and transparency of your spine surgeon, and testimonial of my patients.
Truth
In this blog, I share the truths about alternatives to spinal fusion and other options. I know this because I have experience with all of them. I fully understand that patients’ top three priorities are:
- They want to be out of pain for good.
- They want a safe surgery.
- They want a quick return to work and normal activities.
That’s why I created Deuk Laser Disc Repair.
Transparency
Regarding transparency, my DLDR surgeries are videotaped and livestreamed on my website with patient consent. Yes, they are somewhat graphic, but not as much as open surgeries or even minimally invasive procedures. They clearly show what you will experience and what happens throughout the process.
What our Patients Say
When it comes to promising a quick return to work and normal activities, I am also proud to have an entire archive of patient testimonials that confirm they are pain-free, had a safe surgery, and returned quickly to their regular routines. You’ll see that they came to me with a variety of spinal pain issues.
Make Your First Move to Pain-Free Living
If you are living in pain, we can help you reclaim your life.
Upload your latest MRI to schedule a one-on-one with me. The team will reach out to you to make that happen—and help you take the first step to a pain-free life.
