By Dr. Ara Deukmedjian, MD
Board-Certified Neurosurgeon, Deuk Spine Institute
Medically reviewed on January 29, 2026
Medical disclaimer: This content is for educational purposes only and does not constitute medical advice. Individual results may vary. Always consult with your healthcare provider about your specific condition and treatment options.
L4–L5 disc herniation is a common cause of lower back pain and sciatica, affecting millions of people each year.1,2 This disc sits in the lower back and carries much of your body’s weight while allowing movement. When it herniates, it can press on the L5 nerve, causing pain that radiates down the leg, weakness, and difficulty walking.
Understanding this condition is key to choosing the right treatment. This guide explains the anatomy, current research, and modern treatment options for L4–L5 disc herniation. Whether your symptoms are new, not improving with conservative care, or you are looking for alternatives to fusion surgery, it is designed to help you make informed decisions and move toward recovery.
Understanding L4-L5 Anatomy and the L5 Nerve Root
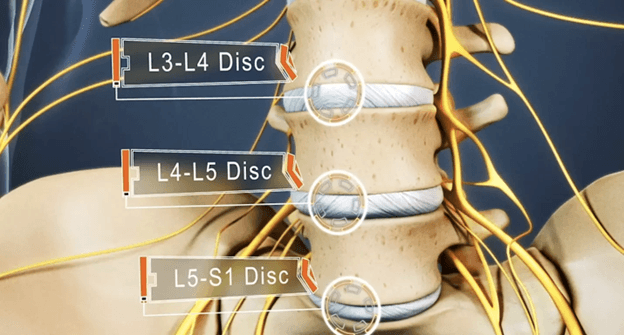
The lumbar spine consists of five vertebrae, labeled L1 through L5, that form the lower portion of your back between your ribcage and pelvis. The L4 and L5 vertebrae sit at the base of your lumbar spine, just above the sacrum, forming one of the most mobile and heavily loaded segments in the entire spinal column.
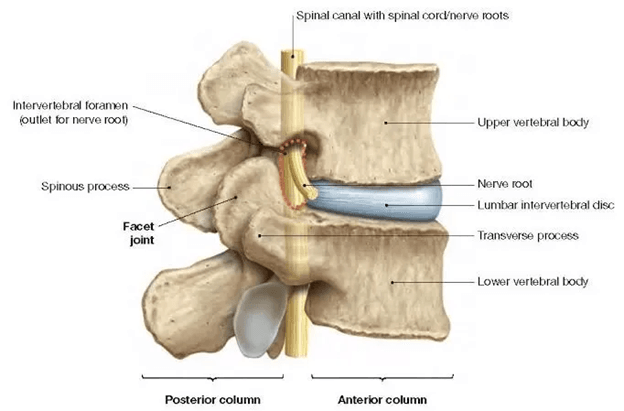
Between each vertebra lies an intervertebral disc that serves as both a shock absorber and a facilitator of movement. Each disc consists of two distinct components:
- Annulus fibrosus: The tough, fibrous outer ring composed of multiple concentric layers of collagen fibers arranged in a crisscross pattern to provide structural strength
- Nucleus pulposus: The soft, gel-like inner core that provides cushioning and distributes compressive forces evenly across the vertebral endplates
A disc herniation occurs when the annulus fibrosus develops a tear or weakness, allowing the nucleus pulposus to protrude beyond its normal boundaries. At the L4-L5 level, this herniated material typically compresses the L5 nerve root as it exits the spinal canal through the neural foramen, a small opening between adjacent vertebrae.
The L5 Nerve Root Distribution
The L5 nerve root controls critical functions throughout the lower extremity, making its compression particularly problematic for mobility and daily activities:3
Motor function (L5 myotome):
- Extensor hallucis longus (extends the big toe upward)
- Tibialis anterior (lifts the foot and ankle, essential for walking)
- Gluteus medius (stabilizes the pelvis during walking)
- Peroneal muscles (control foot eversion and prevent foot drop)
Sensory function (L5 dermatome):
- Lateral aspect of the lower leg
- Top of the foot (dorsum)
- First web space between the big toe and the second toe
- Sometimes portions of the lateral thigh and buttock
Understanding this distribution pattern is crucial because the specific symptoms you experience can help confirm whether the L5 nerve root is the source of your pain and functional limitations.
How Disc Herniation Occurs at L4-L5
The L4–L5 disc is the most commonly herniated disc in the lower back, accounting for about 45–50% of lumbar disc herniations. This is because it sits in a high-stress area of the spine where movement and load are greatest.
This level acts as a transition between the flexible lumbar spine and the more rigid sacrum, exposing it to repeated strain during daily activities. The disc is naturally weaker in the back and side areas where most herniations occur, making it more prone to injury.
Recent research shows that pain from a disc herniation is primarily caused by inflammation around the nerve.4 When disc material leaks out, it triggers an inflammatory response that irritates nearby nerves, contributing significantly to pain and neurological symptoms.
Types of Disc Herniation
Understanding the classification of your disc herniation is important because it influences treatment decisions and prognosis:
- Disc bulge: The entire disc circumference extends beyond the vertebral margins, but the annulus remains structurally intact. This typically represents early degenerative changes rather than a true herniation.
- Disc protrusion: The nucleus pulposus pushes against the weakened annulus but remains contained within it. The base of the herniation is wider than the displaced portion.
- Disc extrusion: The nucleus pulposus breaks through the annulus fibrosus but remains connected to the parent disc. The displaced portion extends beyond the base.
- Disc sequestration: A fragment of the nucleus pulposus completely separates from the parent disc, becoming a free-floating piece in the spinal canal. This is the most severe form, but paradoxically, it may have favorable outcomes with conservative treatment because the immune system can resorb the detached fragment.
Causes and Risk Factors
L4-L5 disc herniation rarely develops from a single event. Instead, it typically evolves through a combination of factors that progressively weaken the disc's structure
Primary Causes
Age-related degeneration: The natural aging process significantly affects intervertebral discs. Beginning in the third decade of life, discs gradually lose water content and proteoglycan molecules, reducing their ability to distribute compressive forces effectively. This process, known as degenerative disc disease, renders the annulus fibrosus more susceptible to tearing. A 2022 study found that the severity of disc degeneration correlates strongly with the likelihood of developing a symptomatic herniation, with moderate to severe degeneration increasing the risk of herniation.5
Acute trauma: Sudden, forceful events can cause immediate disc rupture. Motor vehicle accidents, falls from height, heavy lifting with poor technique, or sports injuries involving spinal flexion and rotation can tear the weakened annulus. However, it's important to understand that even when trauma triggers a herniation, the disc typically has pre-existing degenerative changes that make it vulnerable.
Repetitive stress and occupational factors: Occupations involving repetitive lifting, bending, twisting, or prolonged sitting place cumulative stress on the L4-L5 disc. Recent research from 2023 examining occupational risk factors found that workers exposed to whole-body vibration, such as truck drivers and heavy equipment operators, had a higher risk of developing L4-L5 disc herniation compared to sedentary office workers.6 The combination of vibration, static loading, and awkward postures creates a particularly harmful environment for disc health.
Biomechanical factors, including poor posture, leg length discrepancies, and muscle imbalances, can create asymmetric loading patterns on the L4-L5 disc. Over years or decades, these imbalances accelerate disc degeneration and increase the risk of herniation.
Risk Factors
Understanding risk factors can help you take preventive measures and contextualize your diagnosis:
- Smoking: Nicotine reduces blood flow to disc tissues and decreases oxygen and nutrient delivery, accelerating degeneration. Research shows smokers have a higher risk of developing symptomatic disc herniation.7
- Obesity: Excess body weight increases the mechanical load on lumbar discs. A 2024 study found that individuals with a BMI over 30 had a higher risk of developing L4-L5 disc herniation compared to those with a normal BMI.8
- Genetic predisposition: Hereditary factors influence disc composition and degeneration patterns. If multiple family members experienced disc problems at relatively young ages, genetic susceptibility may be a factor.
- Physical inactivity: Weak core muscles provide inadequate spinal support, increasing stress on intervertebral discs. Regular exercise strengthens supporting musculature and maintains disc health.
- Previous lower back injury: Prior lumbar trauma can increase the risk of future disc problems, even if the initial injury seemed to heal completely.
L4-L5 Herniated Disc Symptoms
Compression and inflammation of the L5 nerve root can produce a distinctive symptom pattern known as L5 radiculopathy. The specific symptoms you experience depend on the degree of inflammation, compression, and individual anatomical variations.
Cardinal Symptoms
- Sciatica radicular leg pain: The hallmark symptom of L4-L5 disc herniation is sciatica, a sharp, burning, or electric-shock-like pain that radiates from the lower back through the buttock, down the lateral thigh and leg, and into the top of the foot. This pain follows the path of the L5 nerve distribution and often intensifies with activities that increase intradiscal pressure, such as sitting, bending forward, coughing, or sneezing. Unlike localized back pain, radicular pain is caused by nerve root inflammation and compression, giving it that characteristic "nerve pain" sensation. 2
- Numbness and paresthesias: Many patients describe a "pins and needles" sensation or frank numbness affecting the lateral lower leg, top of the foot, and the web space between the big toe and second toe. This sensory disturbance may be constant or intermittent and often worsens at night or after prolonged sitting.
- Muscle weakness: When nerve compression is severe enough to affect motor function, specific weakness patterns emerge. The most concerning manifestation is foot drop, an inability to lift the front of the foot during walking caused by weakness in the tibialis anterior muscle. You might notice your foot slapping down when you walk or difficulty clearing your toes when climbing stairs. Weakness in the big toe extensors is also common; you may struggle to push your big toe upward against resistance. These motor deficits, if prolonged, can lead to permanent muscle atrophy.
- Localized lower back pain: While radicular symptoms often dominate the clinical picture, many patients also experience significant lower back pain centered around the L4-L5 segment. This pain results from inflammation within the torn annulus fibrosus and can range from a dull, persistent ache to sharp, stabbing sensations. Recent research has clarified that the outer third of the annulus fibrosus contains sensory nerve endings that, when irritated by inflammatory proteins leaking from the nucleus pulposus, generate intense pain signals.9
- Muscle spasms: Involuntary muscle contractions in the lower back and buttock muscles often accompany L4-L5 disc herniation. These spasms represent your body's attempt to splint and protect the injured segment but can be intensely painful and limiting.
Clinical Insights from Dr. Ara Deukmedjian, MD
Throughout my career performing spine surgery, I've treated thousands of patients with L4-L5 disc herniation. What strikes me most is not just the physical pain these patients endure, but the profound impact on their lives.
I recall one patient, a 52-year-old construction foreman, who came to me after eight months of progressively worsening symptoms. He described how the constant burning pain down his leg made it impossible to stand for more than 15 minutes, forcing him to take medical leave from a job he'd held for 27 years. The numbness in his foot affected his balance, and he'd fallen twice. The weakness in his ankle made it difficult to drive safely, limiting his independence.
What struck me most was when he said, "Doc, I'm not just losing my ability to work. I'm losing who I am. I can't play with my grandkids, I can't help my wife around the house, and I can't sleep through the night. This herniated disc has stolen my life."
This is the reality for many patients with L4-L5 disc herniation. The symptoms extend far beyond physical discomfort, fundamentally altering your ability to work, care for your family, exercise, and maintain your independence. This is why accurate diagnosis and timely, appropriate treatment are absolutely crucial.
Symptom Patterns and Progression
It's important to recognize that L4-L5 disc herniation symptoms can evolve over time. Some patients experience a sudden onset of severe symptoms following a specific injury, while others describe a gradual progression over weeks or months. Understanding these patterns helps distinguish a disc herniation from other conditions.
Additionally, L4-L5 disc herniation symptoms can sometimes be confused with other conditions:
- Hip arthritis or bursitis
- Peripheral artery disease
- Piriformis syndrome4
- Spinal stenosis
- Sacroiliac joint dysfunction
A comprehensive evaluation, including detailed neurological examination and appropriate imaging, is essential for accurate diagnosis. If you've been given a diagnosis that doesn't fully explain your symptom pattern, or if treatments haven't been effective, seeking evaluation from a spine specialist is warranted.
The Importance of Accurate Diagnosis
Accurate diagnosis represents the foundation of effective treatment for L4-L5 disc herniation. Without proper identification of the pain generator and understanding of the specific pathology involved, treatment efforts may be misdirected, prolonging suffering and potentially leading to unnecessary interventions.
Clinical Examination
The diagnostic process begins with a thorough history and physical examination. Your physician should ask detailed questions about the onset and progression of symptoms, the specific distribution of pain and numbness, factors that worsen or alleviate symptoms, the impact on daily activities and sleep quality, previous treatments and their effectiveness, and the presence of concerning symptoms like progressive weakness or bowel/bladder changes.
The physical examination includes specific provocative tests designed to identify nerve root compression:
- Straight leg raise test: While lying on your back, the examiner raises your affected leg with the knee straight. Reproduction of your leg pain (not just back pain) at less than 60 degrees of elevation suggests L5 or S1 nerve root tension. A positive test on the opposite leg (crossed straight leg raise) is even more specific for a disc herniation.
- Neurological examination: A systematic assessment includes motor strength testing in specific muscle groups (particularly toe extensors, ankle dorsiflexors, and hip abductors), sensory examination throughout the L5 dermatome, deep tendon reflexes (though the L5 nerve root doesn't have a reliable reflex), and gait analysis to identify foot drop or compensatory patterns.
The Value of Advanced Imaging
While clinical examination provides valuable information, imaging studies are essential for confirming the diagnosis and guiding treatment decisions.
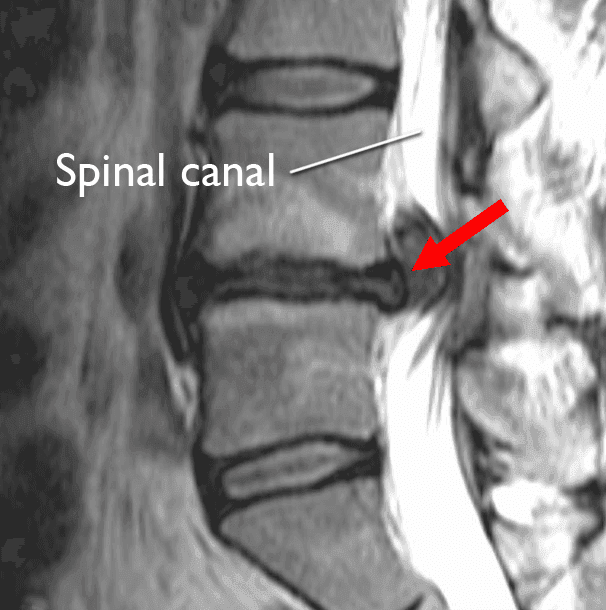
- Magnetic Resonance Imaging (MRI): MRI is the gold standard for diagnosing L4-L5 disc herniation. This technology provides exquisite detail of soft tissues, including the intervertebral discs, nerve roots, and surrounding structures. MRI can reveal the precise location and size of the disc herniation, the degree of neural compression, the presence of annular tears, other degenerative findings at adjacent levels, and spinal canal dimensions.
A critical point that cannot be overstated: not all disc abnormalities seen on MRI are symptomatic. Research consistently shows that a significant percentage of asymptomatic individuals have disc bulges or even small herniations on MRI. This is why correlation between imaging findings and clinical symptoms is essential. Your physician must determine whether the imaging findings explain your specific symptom pattern.
- X-rays: While X-rays cannot directly visualize disc herniation, they provide important information about vertebral alignment, disc space height (significant narrowing suggests advanced degeneration), the presence of spondylolisthesis (vertebral slippage), and overall lumbar spine curvature.
- CT scan: Computed tomography offers excellent visualization of bony structures and may be valuable when X-rays suggest abnormalities requiring further evaluation, MRI is contraindicated, or assessment of bony foraminal stenosis is needed.
- Electrodiagnostic studies (EMG/NCS): Electromyography and nerve conduction studies can help confirm the presence and severity of nerve root compression, identify the specific nerve root affected, distinguish radiculopathy from peripheral nerve problems, and assess the chronicity of nerve damage. These studies are particularly valuable when clinical or imaging findings are ambiguous.
The Second Opinion Advantage
After 20 years in spine surgery, I have learned that getting a second opinion before invasive treatment is often essential. There are many surgical options for spine conditions, and the right choice can significantly affect long-term health and quality of life.
I frequently see patients told they need major fusion surgery when a less invasive option would be effective. I have also seen patients undergo surgery when their condition should have been treated conservatively or with a different approach.
Surgeons differ in their training and perspectives, which influence their recommendations. Those trained primarily in fusion techniques may favor that approach, while minimally invasive specialists can offer options that preserve spinal structure and function.
At Deuk Spine Institute, our focus is on relieving pain while preserving as much natural spinal anatomy as possible, often leading to treatment recommendations that differ from traditional surgery.
Upload Your MRI for Expert Review
If you've been diagnosed with L4-L5 disc herniation and told you need surgery, or if conservative treatments haven't provided adequate relief, I strongly encourage you to seek expert evaluation of your imaging studies. At Deuk Spine Institute, we offer complimentary MRI reviews and virtual consultations. 
You can upload your latest MRI images securely through our website, and my team will reach out to schedule a virtual consultation and review. This service is provided at no cost and comes with no obligation. The goal is simply to ensure you understand all of your treatment options before making one of the most important medical decisions of your life.
Conservative Treatment Approaches
For most patients with L4-L5 disc herniation, an initial trial of conservative (non-surgical) treatment is appropriate. Research indicates that a substantial percentage of patients experience significant improvement with comprehensive conservative management, though success rates vary depending on herniation characteristics and individual factors.10
First-Line Therapies
- Physical therapy: A structured physical therapy program tailored to your specific condition forms the cornerstone of conservative treatment. A qualified physical therapist can design a program incorporating core stabilization exercises to strengthen the muscles supporting your lumbar spine McKenzie Method exercises may help reduce leg symptoms. Gentle stretching can help improve flexibility and reduce muscle tension, and postural training can minimize provocative stresses on the L4-L5 disc.
Recent research from 2024 examining physical therapy outcomes for lumbar disc herniation found that patients who completed a comprehensive program including both directional preference exercises and core stabilization had significantly better outcomes than those receiving passive modalities alone.11 The key is active participation and progressive exercise, not just passive treatments.
- Medications: Various medications can help manage symptoms during the healing process, though they don't address the underlying disc pathology. Non-steroidal anti-inflammatory drugs like ibuprofen or naproxen reduce inflammation around the compressed nerve root, though prolonged use carries risks of gastrointestinal bleeding, cardiovascular events, and kidney dysfunction. Neuropathic pain medications such as gabapentin or pregabalin specifically target nerve pain and may be more effective than traditional analgesics for radicular symptoms. Muscle relaxants can help reduce painful spasms during the acute phase. Oral corticosteroids may provide short-term relief through powerful anti-inflammatory effects, though evidence for long-term benefit is limited.
It's crucial to understand that while medications can provide symptomatic relief, they do not heal the herniated disc or reverse the underlying pathology. They should be viewed as adjuncts to facilitate participation in active rehabilitation, not as definitive treatments.
- Activity modification: Making intelligent adjustments to daily activities can facilitate healing and prevent symptom exacerbation. This includes avoiding prolonged sitting, which significantly increases intradiscal pressure, using proper lifting mechanics and avoiding heavy loads during the acute phase, taking frequent breaks from static postures, and modifying sleeping positions to reduce spinal stress.
Interventional Pain Management
When first-line conservative therapies provide insufficient relief, interventional procedures may be considered:
- Epidural steroid injections: These procedures deliver corticosteroids directly into the epidural space surrounding the compressed nerve root. The anti-inflammatory medication can reduce nerve irritation and provide temporary relief, potentially allowing more effective participation in physical therapy. However, research on long-term efficacy is mixed, and repeat injections can carry increasing risks, including elevated blood sugar in diabetics, bone density loss with frequent use, and, rarely, infection or bleeding.
- Selective nerve root blocks: These diagnostic and therapeutic injections target a specific nerve root, providing both pain relief and confirmation that the suspected nerve root is indeed the pain generator.
It's important to maintain realistic expectations about these interventions. They typically provide temporary symptom relief rather than definitive solutions. If symptoms return after the medication wears off, it indicates the underlying disc pathology remains unaddressed.
Duration of Conservative Treatment
A common question patients ask is: how long should I continue conservative treatment before considering surgery? The answer depends on several factors, including symptom severity and functional impact, rate of improvement with conservative measures, the presence and progression of neurological deficits, and your personal tolerance for ongoing symptoms.
Many spine specialists recommend at least 6-12 weeks of comprehensive conservative treatment before considering surgical intervention, provided no alarming neurological signs are present. However, if you're experiencing progressive weakness, particularly foot drop, earlier surgical consultation may be warranted to prevent permanent nerve damage.
When Surgery Becomes Necessary
While many L4-L5 disc herniations improve with conservative treatment, certain situations warrant surgical intervention to prevent permanent damage and restore quality of life.
Clear Indications for Surgery
- Progressive neurological deficit: If you're experiencing increasing weakness in your leg or foot despite conservative treatment, surgery should be considered promptly. Progressive foot drop is particularly concerning because prolonged compression of the L5 nerve root can lead to permanent muscle atrophy and functional disability. Research shows that outcomes for foot drop improve significantly when decompression surgery is performed within 6-12 months of symptom onset.
- Cauda equina syndrome: This represents a surgical emergency. If your disc herniation compresses multiple nerve roots in the cauda equina (the bundle of nerves at the base of the spinal canal), you may develop bowel or bladder dysfunction, saddle anesthesia (numbness in the perineal region), or bilateral leg weakness. These symptoms require immediate surgical decompression to prevent permanent dysfunction.
- Severe, intractable pain: Pain that significantly impairs your quality of life, prevents you from working or caring for yourself, and doesn't respond to comprehensive conservative treatment (including physical therapy, appropriate medications, and possibly epidural injections) may warrant surgical consideration even without progressive weakness.
- Failed conservative treatment: If you've undergone an appropriate trial of conservative care without adequate improvement, surgery becomes a reasonable option. The definition of "adequate improvement" is subjective and depends on your functional goals and pain tolerance, but generally means you can't perform essential daily activities or maintain employment.
Treatment Options: From Traditional Surgery to Advanced Minimally Invasive Approaches
If surgery becomes necessary for your L4-L5 disc herniation, understanding the available options is crucial for making an informed decision that aligns with your goals and values.
Traditional Surgical Approaches
- Microdiscectomy: This has been the traditional "gold standard" for surgical treatment of lumbar disc herniation. The surgeon accesses the spine through an incision in the lower back, moves aside muscles, removes a portion of the lamina (laminectomy), and excises the herniated disc material compressing the nerve root.
While microdiscectomy can successfully relieve leg pain in many cases, it has several limitations. It requires significant muscle dissection and retraction, potentially causing postoperative pain and weakness. Removal of bone (laminectomy) can destabilize the spine. The procedure doesn't address the underlying annular tear, leading to reherniation rates of 5-15%.12 Additionally, recovery typically requires 6-12 weeks before returning to normal activities.
- Spinal fusion: Some surgeons recommend fusion in conjunction with discectomy, particularly if there's concern about instability or if significant bone removal is necessary for decompression. Fusion permanently connects two vertebrae using bone graft and hardware (screws and rods).
The problems with fusion are substantial and well documented in the literature. It permanently eliminates motion at the fused segment, fundamentally altering spinal biomechanics. Studies show that fusion increases stress on adjacent disc levels, accelerating their degeneration, a phenomenon called adjacent segment disease.
Research indicates up to 25-30% of fusion patients develop symptomatic adjacent segment disease requiring revision surgery within 10 years.13 Recovery is lengthy, often 3-6 months for bone fusion to occur. The procedure is expensive, with costs ranging from $50,000 to over $500,000 depending on complexity and location.
Deuk Laser Disc Repair®: A Revolutionary Approach
After witnessing the limitations and complications of traditional spine surgery throughout my training and practice, I became convinced that a fundamentally different approach was needed. This conviction led to the development of Deuk Laser Disc Repair® (DLDR), a procedure that rethinks how we treat disc herniation at its most basic level.14
- A different philosophy: Traditional surgery operates on a simple premise: remove the herniated disc material, and either fuse the vertebrae or continue with standard discectomy.
DLDR® takes an entirely different approach grounded in the understanding that the disc's outer annulus contains the nerve endings responsible for pain. We precisely remove only the damaged portion of disc material, using laser technology to preserve the healthy disc structure and biomechanics, while minimizing tissue trauma through an endoscopic approach.
- How Deuk Laser Disc Repair® works: DLDR® is performed through a tiny 4-7mm incision in the lower back. Through this minimally invasive opening, a specialized endoscope provides high-definition visualization of the surgical field. Using advanced laser technology the herniated disc material compressing the nerve root is precisely targeted. The laser also ablates inflammatory tissue to further promoting healing.
Because the majority of the disc remains intact and functional, there's no need for fusion, bone removal, or hardware implantation. The natural disc continues to provide cushioning and normal spinal motion. The entire procedure typically takes 30 minutes.
- The science of precision: The key to DLDR®'s remarkable success lies in its precision and respect for anatomy. Traditional surgery requires large incisions, muscle stripping, and often significant bone removal. These approaches are inherently traumatic to surrounding tissues, explaining the prolonged recovery and potential complications of traditional methods.
This precision translates directly into patient outcomes. In over 2,700 patients treated with DLDR® for lumbar disc herniation, we've achieved a patient reported 99.6% success rate with no major or minor complications. Patients typically experience immediate relief from leg, neck, and back pain and return to normal activities within days, not months.
Real Patient Success: A Story of Recovery
Robert, a 48-year-old from Florida, came to Deuk Spine Institute after suffering from an L4-L5 disc herniation for over a year. He had tried physical therapy, multiple epidural injections, and various medications without lasting relief. The burning pain down his left leg was so severe that he could barely walk from his car to his office. He was developing foot drop, making it difficult to drive safely.
After reviewing his MRI, I determined he was an excellent candidate for DLDR®. We performed the procedure on a Friday morning. Robert described his experience: "When I woke up, the leg pain that had tortured me for a year was just... gone. I couldn't believe it. They had me walking within an hour, and I went home that same day. By Monday, I was back at my desk. Within two weeks, I was exercising again. It felt like I got my life back."
Six months later, Robert reported complete resolution of his symptoms, full return to all activities, including golf and jogging, no restrictions on daily activities, and no need for pain medications. His story represents the typical outcome we see with DLDR® for appropriate candidates.
Living with L4-L5 Disc Pain: Practical Management Strategies
While pursuing definitive treatment, implementing practical strategies can help you manage symptoms and potentially prevent worsening.
Exercise and Physical Activity
Appropriate exercise can be beneficial, but selecting the right activities is crucial:
Recommended activities:
- Walking: Low-impact cardiovascular exercise that promotes circulation without excessive spinal loading
- Swimming or water aerobics: Buoyancy reduces gravitational stress on the spine
- Stationary cycling: Cardiovascular conditioning with minimal spinal stress (adjust seat and handlebars for upright posture)
- Gentle yoga or tai chi: Promotes flexibility and core strength with controlled movements
Lumbar-specific exercises:
- Core stabilization: Planks, bird-dogs, and dead bugs strengthen supporting musculature
- Pelvic tilts: Gentle movements that maintain lumbar flexibility
- Knee-to-chest stretches: Can help relieve muscle tension (perform gently)
- Cat-cow stretches: Promotes spinal mobility when tolerated
Activities to avoid:
- High-impact activities like running or jumping
- Heavy weight lifting, especially deadlifts and squats with heavy loads
- Contact sports or activities with twisting motions
- Prolonged forward bending activities, like gardening or repeated toe-touching
Optimizing Sleep Position
Poor sleeping positions can significantly aggravate L4-L5 disc herniation symptoms. Implementing proper sleep ergonomics is essential:
- Back sleeping (often optimal): Place a pillow under your knees to maintain the natural lumbar curve and reduce disc pressure. This position distributes weight evenly and maintains neutral spinal alignment.
- Side sleeping (acceptable with modifications): Place a pillow between your knees to maintain pelvic alignment and prevent lumbar spine rotation. Consider using a full-body pillow for additional support.
- Stomach sleeping (avoid): This position forces lumbar extension and cervical rotation, placing maximum stress on spinal structures. It's the worst possible position for disc problems.
- Mattress considerations: A medium-firm mattress typically provides optimal support. Mattresses that are too soft allow excessive sagging, while those that are too firm create pressure points and don't accommodate natural spinal curves.
Ergonomics and Daily Activities
Modern lifestyle factors often contribute to disc stress. Addressing these can reduce symptom severity:
- Sitting posture: Use a chair with proper lumbar support, position your feet flat on the floor or footrest, take standing breaks every 30-45 minutes, and consider a standing desk for part of your workday.
- Lifting technique: When you must lift, bend at your knees and hips, not your back, keep the object close to your body, avoid twisting while holding a load, and engage your core muscles before lifting.
- Driving: Adjust your seat to maintain lumbar support, position yourself close enough to the pedals to avoid reaching, use cruise control on long trips to vary your posture, and take breaks every hour on extended drives.
Frequently Asked Questions (FAQs)
Q: How serious is an L4-L5 disc herniation?
A: The severity of an L4–L5 disc herniation depends on how large it is, where it’s located, and how much it presses on nearby nerves. Some people experience mild, temporary pain that improves with conservative treatment in a few weeks. Others may develop ongoing pain, weakness, and limits to daily activities.
More serious cases involve worsening nerve problems, such as increasing leg weakness, foot drop, or rare conditions like cauda equina syndrome, which requires emergency care. Symptoms like spreading numbness, loss of bowel or bladder control, or weakness in both legs need immediate medical attention.
The good news is that most people recover well with proper diagnosis and treatment. The key is monitoring symptoms closely and seeking further care if conservative treatment isn’t helping, to prevent lasting nerve damage.
Q: Can an L4-L5 disc herniation heal on its own?
A: Yes, many L4–L5 disc herniations improve without surgery, though the disc itself does not fully “heal” in the traditional sense. Studies show that about 60–70% of patients experience significant symptom relief within 6–12 weeks using conservative treatment.
Improvement happens because the body gradually reduces inflammation, absorbs portions of the herniated disc material, and decreases nerve irritation. Even if some disc bulge remains, pain and nerve symptoms often lessen as swelling subsides and the body adapts.
However, symptom relief does not mean the disc returns to normal. The disc remains structurally damaged and may show degeneration on imaging, which is why symptoms can recur later. Ongoing prevention and spine care remain important.
If symptoms last beyond 8–12 weeks, worsen, cause increasing weakness, or significantly affect daily life, a surgical evaluation may be appropriate.
Sources
1: https://www.hopkinsmedicine.org/health/conditions-and-diseases/lumbar-disc-disease-herniated-disc
2: https://deukspine.com/blog/what-is-causing-my-sciatica
3: https://pmc.ncbi.nlm.nih.gov/articles/PMC4300884/
4: https://pmc.ncbi.nlm.nih.gov/articles/PMC8966871
5: https://www.ncbi.nlm.nih.gov/books/NBK560878
7: https://www.scirp.org/journal/paperinformation?paperid=149023
8: https://pubmed.ncbi.nlm.nih.gov/38363366
9: https://www.wjgnet.com/2218-5836/full/v16/i1/102120.htm
10: https://pmc.ncbi.nlm.nih.gov/articles/PMC11465477
11: https://pmc.ncbi.nlm.nih.gov/articles/PMC10888666
12: https://pmc.ncbi.nlm.nih.gov/articles/PMC4430997
13: https://www.sciencedirect.com/science/article/pii/S2772529425001511
14: https://deukspine.com/treatment-options/deuk-laser-disc-repair