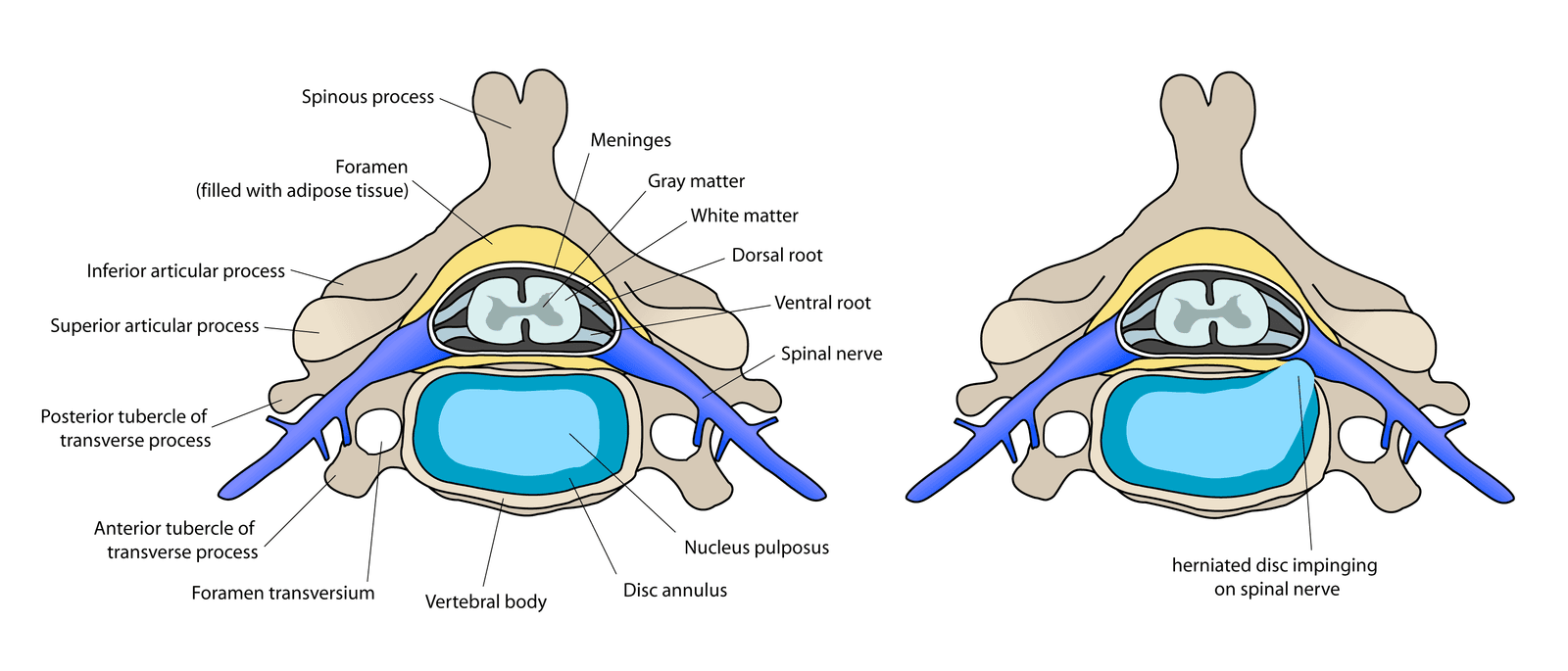
Deciding to undergo surgery involving your neck and spine can be a daunting experience filled with questions and concerns. One of the most common procedures for neck pain and nerve compression is the Anterior Cervical Discectomy and Fusion, or ACDF. This surgery is often recommended for conditions such as herniated discs, degenerative disc disease, and cervical stenosis. If ACDF has been recommended for your condition, your first question is likely to be, "Is it safe?"
It's Complicated
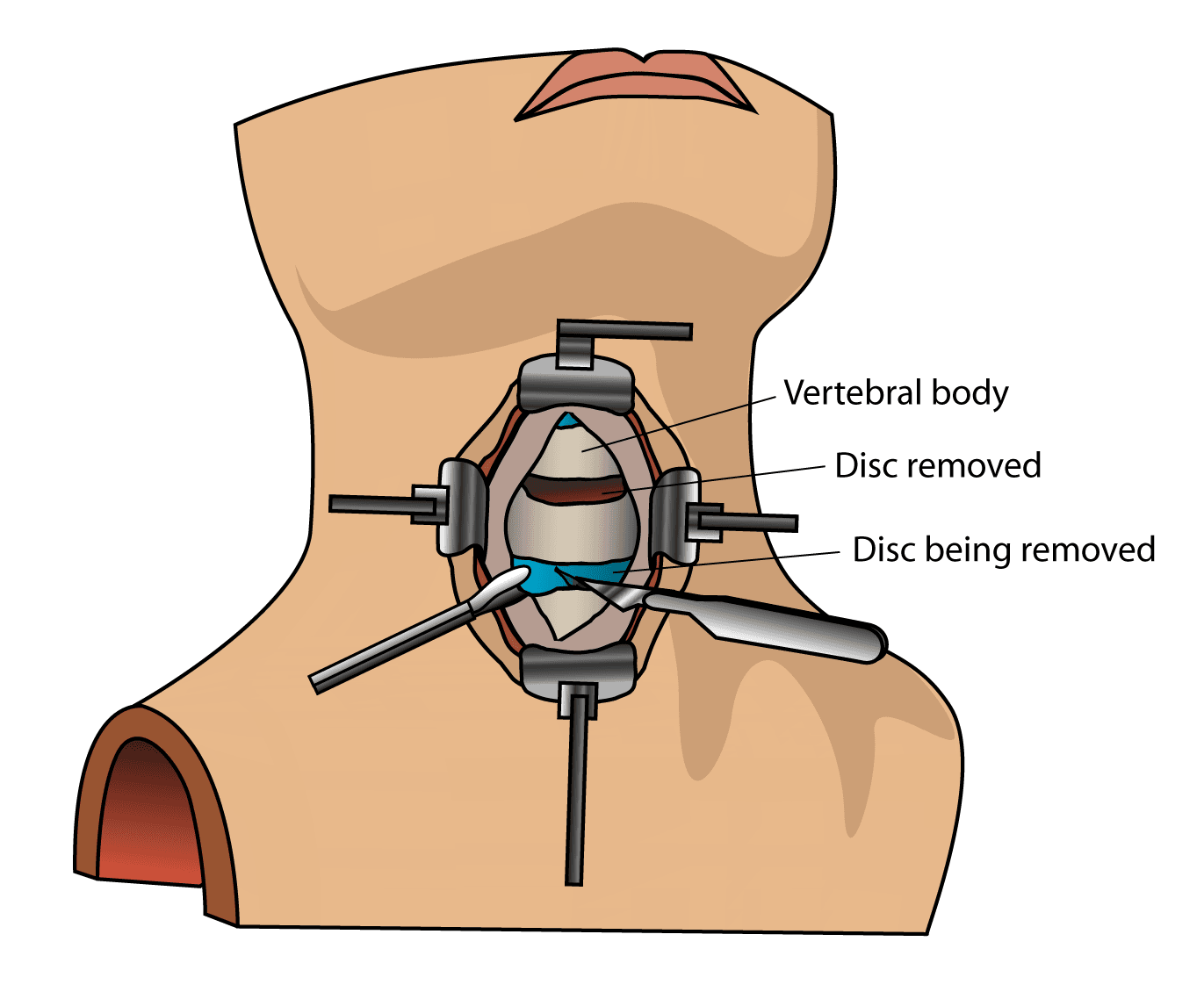
ACDF is a highly invasive surgery that starts with a large incision at the front of your neck to directly reach the vertebrae and discs. The surgeon must navigate through a complex network of front-facing structures, such as the trachea, esophagus, carotid artery, jugular vein, recurrent laryngeal nerves, vagus nerve, and the longus coli muscles, just to access the cervical spine. It’s an intricate approach, so there are several potential complications.
The higher the number of levels, the higher the risk of complications:
- 1-level ACDF: 20.5%
- 2-level ACDF: 20.3%
- 3-level ACDF: 28.0%
- 4-level ACDF: 53.0%
The Top 11 Risks
There are 11 main risks associated with ACDF surgery:
- Hoarseness (Dysphonia)
Recurrent laryngeal nerve (RLN) injury is the most common cause of dysphonia after ACDF. The recurrent laryngeal nerves branch off the vagus nerve and control the movement of the vocal cords. During ACDF surgery, these nerves are directly in the surgeon’s path to reaching the spine. RLN injury can cause vocal cord paresis or paralysis, leading to symptoms such as hoarseness, a breathy voice, or a weak voice. These nerves are at risk of injury during surgery due to
- Stretching or traction: The surgeon uses retractors to hold the neck tissues, including the trachea and esophagus, out of the way to access the spine. This can stretch or press on the recurrent laryngeal nerves, a condition known as neuropraxia.
- Direct surgical trauma: Although less common, direct injury to the nerve can happen from cutting, ligating (tying off), or other surgical maneuvers.
- Post-operative swelling: Swelling or hematoma (a collection of blood) in the area after surgery can compress the nerve, causing temporary or, in rare cases, permanent dysfunction.
2. Difficult and Painful Swallowing (Dysphagia and Odynophagia)
The esophagus, or swallowing tube, and trachea (windpipe) are located directly in front of the cervical spine. To access the spine, the surgeon must gently move these structures aside. This "retraction" of the soft tissues can cause inflammation and swelling in the throat, leading to difficult swallowing (dysphagia) and painful swallowing (odynophagia). Other possible causes include:
- Mechanical Irritation: In some rare cases, the surgical hardware (plate and screws) can press against the esophagus, causing an obstruction.
- Nerve Damage: Although rare, damage to the nerves that control the muscles of the throat and swallowing can also occur.
These injuries can be permanent. Patients may even need a nasogastric (NG) or percutaneous endoscopic gastrostomy (PEG) tube to feed them for weeks after surgery.
3. Permanent Nerve Damage
ACDF surgery can directly and indirectly damage the longus colli muscle, a long, thin muscle located on the front surface of the cervical vertebrae, extending from the first cervical vertebra (C1) down to the third thoracic vertebra (T3). It is part of the deep cervical flexor muscles, which are essential for neck movement and stability.
The longus colli is closely associated with several important nerves, particularly the sympathetic trunk, which runs over the muscle's surface. The sympathetic trunk is responsible for many involuntary functions. Damage to this nerve chain during retraction of the longus colli can lead to Horner's syndrome, a rare but known complication of anterior cervical surgery. This condition is characterized by a droopy eyelid (ptosis), constricted pupil (miosis), and decreased sweating on one side of the face (anhidrosis).
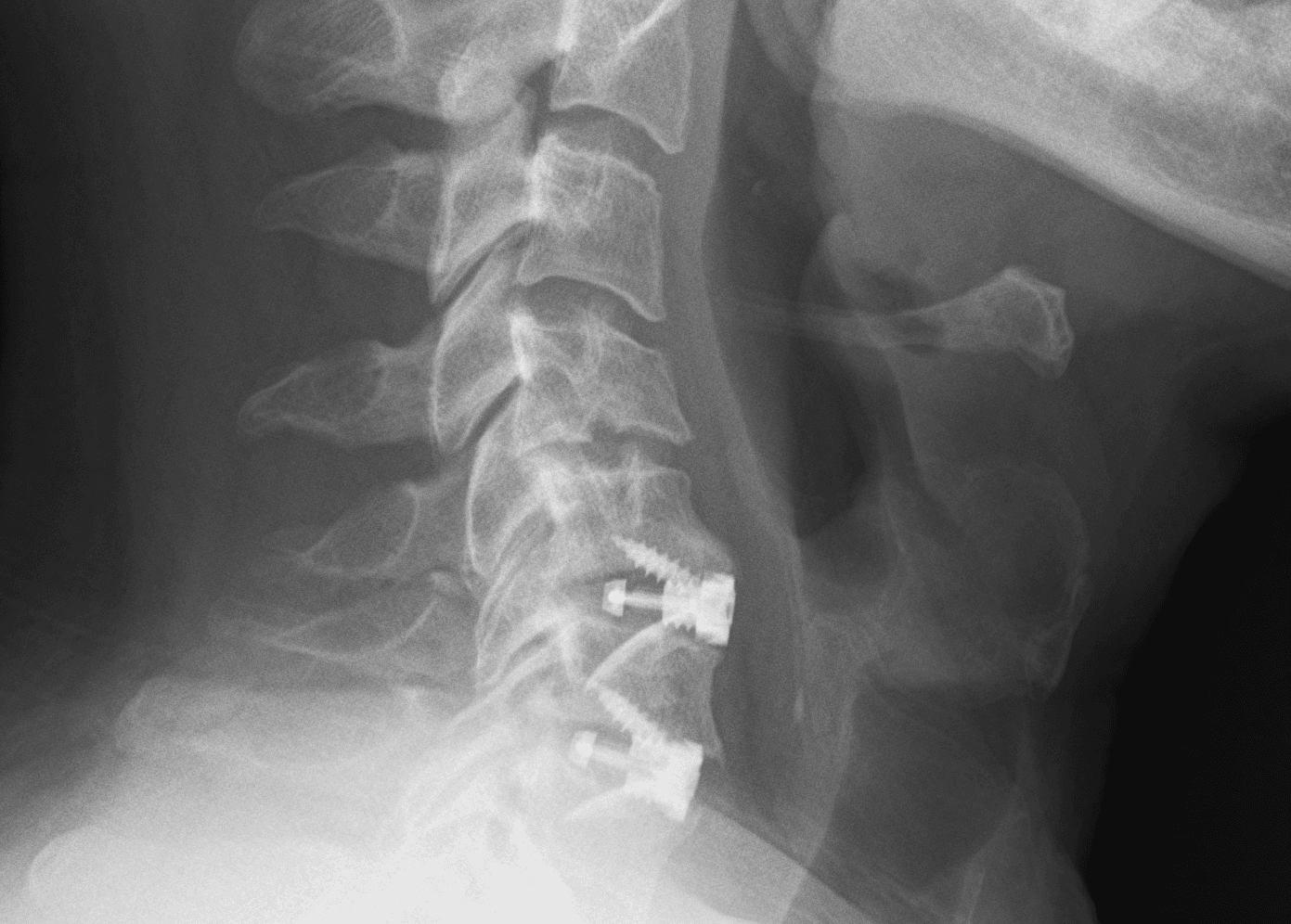
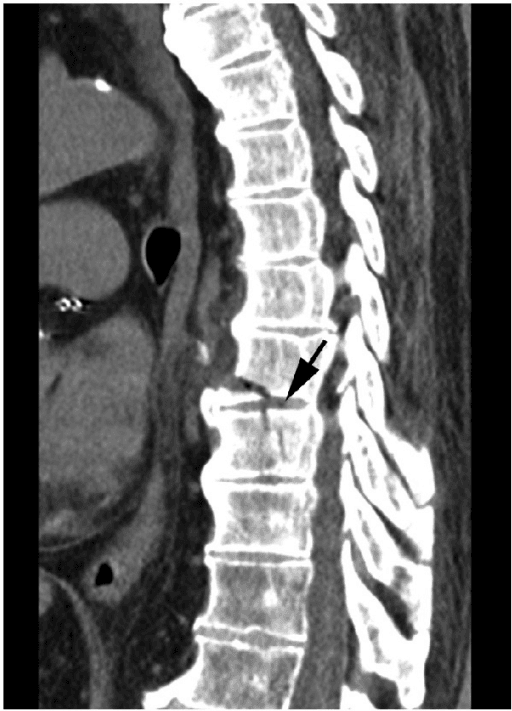
4. Endplate Fracture
An endplate fracture is a break in the bony endplate of a vertebra. In the context of ACDF, it can occur during the surgical procedure, especially when preparing the vertebral endplates for the placement of a bone graft or cage. This fracture can be caused by:
- Over-preparation: Excessively removing the endplate during surgery can weaken the bone, making it more prone to fracture. The aim of endplate preparation is to expose the vascular cancellous bone to promote fusion, but removing too much of the hard cortical bone can increase the risk of the cage or graft sinking into the vertebral body, a complication called "subsidence."
- Screw Penetration: Driving a screw too close to or through the endplate can cause a fracture.
- Pre-existing conditions: Patient factors can elevate the risk of endplate fracture. Osteoporosis, for example, weakens the bone, making it more fragile and prone to breakage fracture.
An endplate fracture can lead to several complications, including:
- Subsidence: This is the most common and significant consequence. Subsidence occurs when the cage or graft sinks into the softer cancellous bone of the vertebral body. This can lead to a loss of disc height, changes in spinal alignment (kyphosis), and potential nerve root compression.
- Non-union (pseudarthrosis): If the endplate is severely damaged, it can hinder the fusion process. The lack of a stable base for the graft can prevent new bone from growing, leading to a "failed fusion."
- Instability: A damaged endplate can compromise the stability of the surgical segment, potentially leading to the loosening or dislodgement of plates and screws.
5. Hardware Failure
Hardware failure can present in various forms, and the resulting injuries depend on the type of failure and the specific location of the hardware.
- Hardware loosening or dislodgement: Screws can loosen over time, and plates or cages can become displaced. This can lead to nerve compression, spinal instability, and dysphagia.
- Hardware breakage: Plates or screws can break due to stress, especially if the fusion does not heal properly, leading to instability, failed fusion, nerve and spinal cord damage, and chronic pain from inflammation.
- Subsidence: This occurs when the bone graft or cage migrates or sinks into the adjacent vertebral bodies, causing nerve compression and loss of spinal alignment
6. Infection (Discitis and Osteomyelitis)
Discitis and osteomyelitis are both serious infections of the spine. They are often discussed together because they frequently occur at the same time, especially after spinal surgery. Here is a breakdown of each condition:
- Discitis is an infection of the intervertebral disc space. The intervertebral discs are soft, cushion-like structures between the vertebrae. Bacteria are introduced directly into the disc space, often as a complication of the ACDF surgical procedure.
- Osteomyelitis is a serious bone infection that, like discitis, is caused by bacteria entering the bone from another infection via the bloodstream, from a nearby infected area, or directly during procedures such as the placement of a plate or screws. A bone infection is serious because it can lead to bone death (osteonecrosis) and the formation of an abscess within the bone, which can put pressure on the spinal cord and nerves. It can also weaken the bone, increasing the risk of fractures.
The main treatment for both conditions is a prolonged course of intravenous (IV) antibiotics, typically lasting four to six weeks or longer. In severe cases or if the infection doesn't respond to antibiotics, surgery may be needed to drain abscesses and remove infected bone and tissue.
7. Spinal Fluid Leak
One of the more serious complications of ACDF is a spinal fluid leak. This happens when the dura, the tough, fibrous membrane that surrounds the spinal cord and contains cerebrospinal fluid (CSF), is accidentally torn or punctured during surgery.
Most dural tears are identified and repaired by the surgeon during the operation. However, a small tear might not be immediately noticeable, especially if the innermost layer of the dura stays intact. These "occult" leaks can appear days, weeks, or even years after surgery.
In some cases, a second surgery may be necessary to repair the tear directly. In others, a temporary lumbar spine drain can be placed to divert CSF and reduce pressure, allowing the tear to heal.
8. Vascular Injury
Due to the proximity of major blood vessels in the neck, vascular injuries, while rare, are a potential and serious concern. Here are the primary vascular injuries that can occur during ACDF surgery:
- Carotid artery injury: The carotid arteries are the major vessels that supply blood to the brain. During an ACDF, they are carefully retracted to allow the surgeon access to the spine. While direct injury is uncommon, complications can arise from the manipulation and retraction of the artery.
- Vertebral artery injury: The vertebral arteries run through the bony tunnels (transverse foramen) of the cervical vertebrae.They are at risk of injury, particularly during the decompression or instrumentation phases of the surgery, such as when using drills or other instruments.
- Jugular vein injury: The internal jugular veins are located alongside the carotid arteries and collect blood from the brain and face. These veins have a delicate wall and can be easily torn during the surgical approach.
- Postoperative hematoma: This is the most common cause of significant bleeding and anemia after ACDF. A hematoma is a collection of blood outside the blood vessels, and in this case, it forms in the neck tissues around the surgical site.
9. Nerve Root Damage
Nerve root damage is permanent. It’s not fixable. Nerve damage during ACDF surgery can occur for a few reasons:
- Direct surgical trauma: There is a risk of accidentally injuring the nerve root with surgical instruments like grasping tools or a drill. This can be more likely in cases with severe stenosis or complex anatomy.
- Nerve stretching (neuropraxia): When the surgeon removes the disc and bone spurs, the compressed nerve root is suddenly decompressed. This sudden relief of pressure can cause the nerve to stretch, leading to a temporary condition called neuropraxia – a feeling of "heaviness," numbness, tingling, or weakness in the arm or hand.
- Post-operative inflammation and swelling: The surgical process itself can cause inflammation and swelling around the nerves, leading to symptoms like pain, numbness, or tingling that may persist for days, weeks, or even months after the surgery.
- Scar tissue formation: In some cases, scar tissue can form around the nerve root during the healing process. This can cause new or recurring compression on the nerve, leading to persistent symptoms.
10. Brain Death
The main ways that ACDF surgery could potentially cause a catastrophic neurological event like brain death are through complications that interrupt blood flow or oxygen to the brain. The mechanisms by which ACDF surgery can lead to a stroke are mainly related to the manipulation of major arteries in the neck that supply blood to the brain, which can cause:
- Stroke: During the surgery, the surgeon works in close proximity to the carotid and vertebral arteries, which supply blood to the brain. While rare, there is a risk of a vascular injury, or a blood clot (thrombus) forming and traveling to the brain, causing an ischemic stroke. A massive stroke that affects a large portion of the brain or the brainstem can be a cause of brain death. Stroke is not always an immediate complication. A dissection of the vertebral or carotid artery may not lead to a stroke until hours or even days after the surgery.
- Airway Compromise: Swelling, a hematoma (collection of blood), or an abscess in the surgical area can compress the trachea (windpipe) or other airway structures. If this happens and is not managed promptly, it can lead to respiratory arrest. When the brain is deprived of oxygen for an extended period, it can suffer irreversible damage, which can lead to brain death. This is one of the most immediate and critical postoperative complications to be aware of.
- Vertebral artery compression or injury: The vertebral arteries run through the cervical spine and supply blood to the brainstem. In extremely rare cases, a hematoma or other injury during surgery could compress or damage a vertebral artery. This can lead to ischemia (lack of blood flow) in the brainstem, which controls vital functions like breathing and consciousness.
11. Respiratory Failure
Respiratory compromise due to ACDF surgery can occur due to a number of factors, primarily related to the surgical approach and the anatomy of the neck.:
- Soft tissue swelling and hematoma: This is the most common cause. The surgery involves an incision in the front of the neck and gentle retraction of structures like the trachea (windpipe) and esophagus to access the spine. This can cause soft tissue swelling (edema) in the neck. In some cases, a hematoma (a collection of blood) can form at the surgical site. Both swelling and hematoma can put pressure on the airway, leading to partial or complete obstruction and making it difficult to breathe.
- Phrenic nerve injury: The phrenic nerve, which controls the diaphragm (the primary muscle of breathing), runs along the front of the cervical spine. It can be injured during the surgical procedure through direct damage, traction, or even stretching. Unilateral phrenic nerve palsy (damage to one side) may not cause significant symptoms if the other side is healthy, but bilateral injury or injury in a patient with pre-existing lung disease can lead to severe respiratory distress and the need for ventilator support.
- Recurrent laryngeal nerve damage: This nerve controls the vocal cords and is located near the surgical site. Injury to this nerve can cause hoarseness or difficulty speaking, and in rare cases, can lead to vocal cord paralysis, which can compromise the airway and cause breathing difficulties.
- Anesthesia and post-operative effects: While rare, complications related to anesthesia can also contribute to respiratory issues. These can include allergic reactions, residual effects of muscle relaxants, or an inability to wean a patient off the ventilator after surgery.
- Spinal cord edema or injury: In rare cases, swelling or injury to the spinal cord itself can affect the nerves that control breathing, leading to respiratory compromise.
DEUK LASER DISK REPAIR (DLDR): No Complications
These risks may seem worth ACDF surgery compared to the horrible pain of a herniated disc, degenerative disc disease or spinal stenosis in the neck. But here’s your alternative - with no complications: Deuk Laser Disc Repair.
It takes less than an hour, and our patients leave the outpatient clinic a few hours after surgery without pain or the need for addictive painkillers. They simply return the next day for a postoperative review.
Our success rate is 99.5%, and we have treated thousands of patients who are now living pain-free. It took 20 years and countless hours of surgery to identify the root cause of chronic back pain and demonstrate the effectiveness of lasers in treating it. View a livestream of a Deuk Laser Disk Repair to treat cervical herniation rather than a ACDF.
Take the First Step to Living Pain Free
Upload your latest MRI for a free review and a personal consultation with me, Dr. Ara Deukmedjian, M.D., founder of Deuk Spine Institute and creator of the Deuk Laser Disc Repair® procedure. Our team will contact you to help you regain your life.
