Anterior Cervical Corpectomy with Fusion (ACCF): Fusion Is The Risk
Anterior Cervical Corpectomy with Fusion, often abbreviated as ACCF, is a complex, invasive surgical technique that addresses serious problems in the cervical spine—the part of your spine that makes up your neck. This article provides a concise overview of ACCF, explaining what it is, the conditions it treats, how it differs from a discectomy, the potential risks and complications involved. The article also recommends Deuk Laser Disc Repair as “the better way” – a less complicated, less than minimally invasive procedure, with a 99.5% success rate that actually cures neck pain - for good.
Discectomy vs Corpectomy: The Difference
A discectomy is focused on the disc. The procedure involves removing a part of a damaged or herniated intervertebral disc that is pressing on a nerve. The procedure's goal is to alleviate the pressure caused by the disc material without removing the adjacent vertebrae.
A corpectomy is a more extensive removal. It involves the removal of an entire vertebral body (the main bone of the spinal column) as well as the discs above and below it. Because a major bone is removed, a corpectomy always requires a spinal fusion to stabilize the spine afterward. ACCF is not a first-line treatment for common neck pain. It is reserved for serious conditions where there is significant compression of the spinal cord or nerve roots, often spanning more than one spinal level. Surgeons may recommend ACCF for:
Cervical Spondylotic Myelopathy (CSM): This is a progressive condition caused by age-related wear and tear on the cervical spine. Arthritis can lead to the formation of bone spurs (osteophytes) and the thickening of ligaments, which narrow the spinal canal and compress the spinal cord. When this compression is extensive and severe, an ACCF may be needed to create adequate space for the cord.
Ossification of the Posterior Longitudinal Ligament (OPLL): This is a condition where a key ligament that runs along the back of the vertebral bodies becomes thick and bone-like. As this ligament calcifies, it expands into the spinal canal, placing severe pressure on the spinal cord. ACCF allows for the direct removal of this compressing bone mass.
How is the Corpectomy a More Extensive Surgery?
ACCF is a procedure involves removing one or more vertebral bodies (the large, block-like parts of the vertebrae) and the adjoining discs. This is done to decompress the spinal cord and nerves. After removing the damaged bone and discs, a void is left. To restore stability, the surgeon fills this space with a structural bone graft. This can be a fibular strut graft (bone from a cadaver) or a synthetic cage packed with bone material. A metal plate and screws are then typically fixed to the vertebrae above and below the gap. Over time, the vertebrae fuse together with the graft, creating a single, solid segment of bone intended to stabilize the spine.

ACCF Complications: From Minor to Serious
As with any major surgery performed close to the spinal cord and nerve roots, ACCF surgical complications can occur, ranging from mild to serious.
Negative Side Affects
Difficulty Swallowing (Dysphagia): This is the most common temporary side effect, occurring in up to half of patients after surgery. Retraction of the esophagus and trachea (windpipe) during the procedure can cause swelling and irritation, leading to a sore throat or a sensation of food getting stuck when swallowing.
Hoarseness (Dysphonia): The recurrent laryngeal nerve, which controls the vocal cords, runs near the surgical field. Temporary hoarseness affects up to 10% of patients, usually resolving within weeks to a few months. However, permanent vocal changes occur very rarely.
Adverse Reactions to Anesthesia: As with any major surgery, complications related to anesthesia can occur, ranging from mild nausea to, very rarely, more serious reactions.
Serious Perioperative Complications
Nerve or Spinal Cord Injury: One of the rarest but most serious complications. Because the surgery is performed close to the spinal cord and nerve roots, there is a small risk (significantly less than 1%) of direct injury, which could lead to new weakness, numbness, loss of sensation, or, in extremely rare cases, paralysis. Any new neurological symptoms after surgery need to be immediately evaluated
Infection: As with any surgical procedure, there is a risk of postoperative infection, although it is uncommon (less than 1–2% of cases). Surgical site infections (SSI) may be superficial (involving only the skin) or, rarely, deep (affecting the bone or hardware). Strict sterilization protocols, prophylactic antibiotics, and careful wound care are used to reduce this risk. Most infections can be managed with antibiotics, but occasionally, further surgery is needed.
Bleeding and Blood Clots: Major bleeding during ACCF is uncommon due to the careful surgical approach, but there is always a risk of blood vessel injury since the neck contains major arteries and veins. Blood loss is usually minimal, and transfusions are rarely needed. Blood clots in the legs (deep vein thrombosis) or lungs (pulmonary embolism) are rare but serious risks. Early mobilization after surgery and the use of compression devices help lower this risk.
Dangerous Mechanical Complications
Many mechanical complications can occur after spinal fusion surgery when an interbody cage (a device placed between vertebrae to restore disc height and promote fusion) is used:
Cage Kick-Out: This happens when the interbody cage migrates or slips out of its intended position - usually backward into the spinal canal or forward into soft tissues like the trachea. It’s often due to poor cage fit, inadequate endplate preparation, incorrect size selection, or instability before fusion takes hold. Cage kick-out can compress nerve roots or the spinal cord, causing pain, weakness, or neurological symptoms.
Cage Telescoping/Subsidence: Subsidence , the most common term, is when the cage sinks into the vertebral endplates instead of staying seated between them. This happens when the bone of the vertebra is weak (osteoporosis) or if the cage is too small or improperly positioned. Leads to loss of disc height and potential nerve compression. Telescoping, the less common term, refers to a situation where one vertebral body collapses downward onto another, with the cage being pressed further in, like a telescope sliding in. It is essentially a type of severe subsidence.
Serious Perioperative Complications
Nerve or Spinal Cord Injury: One of the rarest but most serious complications. Because the surgery is performed close to the spinal cord and nerve roots, there is a small risk (significantly less than 1%) of direct injury, which could lead to new weakness, numbness, loss of sensation, or, in extremely rare cases, paralysis. Any new neurological symptoms after surgery need to be immediately evaluated
Infection: As with any surgical procedure, there is a risk of postoperative infection, although it is uncommon (less than 1–2% of cases). Surgical site infections (SSI) may be superficial (involving only the skin) or, rarely, deep (affecting the bone or hardware). Strict sterilization protocols, prophylactic antibiotics, and careful wound care are used to reduce this risk. Most infections can be managed with antibiotics, but occasionally, further surgery is needed.
Bleeding and Blood Clots: Major bleeding during ACCF is uncommon due to the careful surgical approach, but there is always a risk of blood vessel injury since the neck contains major arteries and veins. Blood loss is usually minimal, and transfusions are rarely needed. Blood clots in the legs (deep vein thrombosis) or lungs (pulmonary embolism) are rare but serious risks. Early mobilization after surgery and the use of compression devices help lower this risk.
Long-term Surgical Complications
Kyphosis: Kyphosis is an abnormal forward curve of the spine that can happen if the cage collapses, sinks, or is positioned incorrectly. When the front part of the spinal column loses height (due to cage failure or vertebral collapse), the segment tilts forward, causing a kyphotic deformity. This deformity can lead to chronic pain, imbalance, and neurological problems, sometimes requiring revision surgery.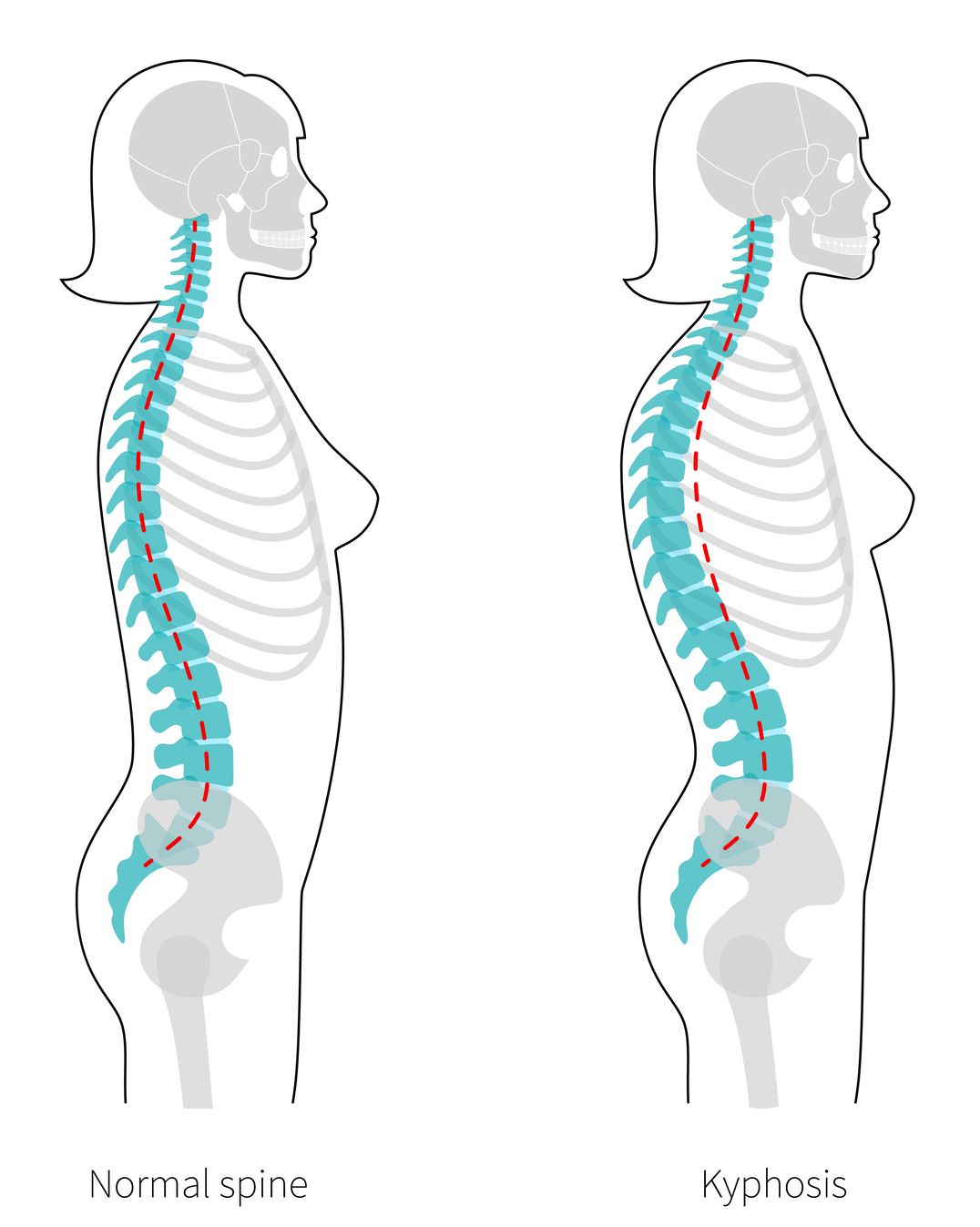
Adjacent Segment Disease: When spinal segments are fused, it reduces movement at those levels but puts extra stress on the vertebrae above and below the fused area. Over time, this may lead to faster degeneration in those neighboring segments—a condition known as adjacent segment disease. This process can take years to develop, and not all patients will experience symptoms. The risk increases with the number of levels fused. Doctors monitor for new symptoms over the years and may suggest physical therapy, medications, or, if necessary, further surgery if serious problems arise.
Deuk Laser Disc Repair: The Better Way
If you are told you need ACCF, you don’t have to undergo this invasive and extensive surgery. The fact that fusion requires hardware placement and can lead to complications makes it a daunting option. You don’t need to choose it. There’s a better solution – Deuk Laser Disc Repair (DLDR), the most advanced laser spine surgery available and a safer alternative to risky, invasive procedures like spinal fusion.
Renowned neurospine surgeon Dr. Ara Deukmejian, M.D., created and performs this groundbreaking procedure that bears his name. DLDR is a form of endoscopic spine surgery done at a modern outpatient surgery center, with the patient under sedation and relaxed. DLDR does not compromise or weaken the spine’s health or integrity. It involves a quarter-inch incision. No cutting or retracting is required, which means no damage to muscles, ligaments, tendons, or blood vessels. It’s a better way.
Watch It Live
Our goal is to be completely transparent about our process and procedures for treating back issues. We livestream surgeries with our patients’ written consent, so you can observe our technique.
Make the First Move to Move Pain-Free
Upload your latest MRI for a free review and a personal consultation with acclaimed spinal surgeon Dr. Ara Deukmedjian, M.D., founder of Deuk Spine Institute and creator of the Deuk Laser Disc Repair® procedure. Our team will contact you to help you regain your life.
