Your doctor says your back pain is due to poor posture. Your chiropractor blames weak core muscles. Your physical therapist attributes it to tight hamstrings. Meanwhile, you've spent six months strengthening your core, improving your posture, and stretching religiously, and your back still hurts every single day. The pain wakes you at night, limits what you can do with your family, and affects your work performance. Nobody has given you a clear explanation of what's actually causing it.
After over 30 years of performing spine surgery, I've learned that most explanations of back pain miss the actual source. Poor posture doesn't cause chronic back pain; in clinical practice, I observe that postural changes often develop as patients adapt to existing pain rather than trying to force it. Weak muscles don't generate the pain signals keeping you awake at night. Damaged discs and inflamed joints do. Through clinical practice and diagnostic refinement, I've identified 30 structurally identifiable sources of chronic lower back pain, and understanding which ones are causing your symptoms determines whether treatment will cure your pain or just temporarily manage it.
Here's what's causing chronic back pain. Here is why accurate diagnosis requires comprehensive evaluation beyond imaging alone.
Defining Chronic Back Pain
Chronic back pain is back pain that persists for more than 2 weeks.

This definition matters because acute back pain (muscle strains from lifting, temporary soreness from unusual activity) resolves naturally within days to two weeks. Chronic back pain that persists beyond two weeks indicates structural problems: damage to discs, joints, or other spinal structures that won't heal on their own without intervention.
The 30 Sources: Disc Injuries Dominate
Through clinical practice and research, I've identified and cataloged 30 specific, structurally identifiable sources of chronic back pain. These aren't vague lifestyle factors. They're anatomical structures that can be seen on imaging and confirmed through physical examination.
Not all 30 sources occur with equal frequency:
Disc injuries account for the majority of chronic back pain cases. Based on my clinical experience performing over 2,700 Deuk Laser Disc Repair® procedures, disc injuries represent approximately 85% of chronic back pain. The lower back contains five discs: L1-L2, L2-L3, L3-L4, L4-L5, and L5-S1. The most common disc to cause back pain is L4-L5, followed by L5-S1, then L3-L4, and finally L2-L3. Pain from disc injuries originates from inflammation in the posterior annular tear, the area where the tough outer disc layer (annulus fibrosus) tears and allows inner disc material (nucleus pulposus) to leak out, triggering inflammatory responses.
Facet joint injuries are the second most common cause. Facet joints are small, weight-bearing joints located behind the discs. There are two facet joints (left and right) for each disc level. Facet joint pain parallels disc pain in frequency. These occur most often at L4-L5, then L5-S1, then L3-L4, then L2-L3.
Sacroiliac joint pain and piriformis muscle pain are the third most common causes. These two sources are roughly equal in prevalence. The sacroiliac (SI) joint connects your pelvis to your spine. The piriformis muscle runs from your sacrum to your hip and can become chronically inflamed from injury.
Vertebral body fractures represent less than 0.5% of chronic back pain. These fractures typically occur from trauma or osteoporosis and are relatively rare compared to disc and joint injuries.
The remaining 25 identified sources include various muscle injuries, ligament strains, nerve entrapments, and other structural problems that individually occur less frequently but collectively account for approximately 5% of chronic back pain cases.
Why Disc Injuries Cause Most Back Pain
Your spinal discs have a tough outer layer (annulus fibrosus) surrounding a soft inner nucleus pulposus. When the disc degenerates or experiences injury, the annulus develops tears, most commonly in the back of the disc (posterior annular tear). Nucleus pulposus material from inside the disc can herniate through this tear.
The herniated material and the damaged tissue surrounding the posterior annular tear trigger an inflammatory response. This inflammation, combined with mechanical stress on pain-sensitive structures in the outer annulus and posterior longitudinal ligament, generates your pain signals. Small pain nerve fibers can grow into the damaged and inflamed area, potentially intensifying the pain over time. This is why disc pain often worsens gradually rather than improving. The inflammatory process can become persistent.
Research published in the American Journal of Neuroradiology demonstrates that annular tears occur in the early stages of disc degeneration and are associated with faster subsequent nuclear degeneration. In a longitudinal study by Sharma et al., annular tears were found in 73.5% of discs examined, with many tears present even in discs with preserved signal intensity, suggesting that annular tears precede obvious nuclear degeneration.
The Critical Distinction: What Actually Causes Your Pain
Most explanations of back pain are fundamentally wrong about pain sources.
Pinched nerves NEVER cause back pain. Nerve compression causes leg pain, numbness, tingling, and weakness, but not back pain itself. When a herniated disc compresses a nerve root, you feel symptoms in your leg (sciatica), not your back. This distinction is well established in the spine literature. Nerve compression produces radicular symptoms along the nerve distribution, while axial back pain originates from disc and joint structures.
Spinal stenosis does NOT cause back pain. Stenosis means narrowing of the spinal canal. This narrowing can compress nerves, causing leg symptoms when walking (neurogenic claudication). But stenosis itself doesn't generate back pain. If you have both stenosis and back pain, the back pain is caused by a disc injury, facet arthritis, or another structural problem. The stenosis itself does not cause the back pain.
Pain can come from disc and facet joint injuries, which can trigger muscle spasms. The muscle spasms you might feel are secondary. This is a protective response to underlying structural injury. Your back muscles spasm because damaged discs or inflamed joints are sending pain signals. The muscles contract to splint and protect the injured area.
This is why muscle relaxants, massage, and stretching don't cure chronic back pain. They address the symptom (muscle spasm) rather than the source (disc or joint injury causing the spasm). When the underlying structural problem remains untreated, symptoms return.
Understanding the Three Types of Spine Pain
1. Axial Disc Pain (Back Pain from Disc Injury)
Axial pain means pain felt in your back at the level of the injured disc. This is the pain from that posterior annular tear with associated disc disruption, causing inflammation and mechanical stress on pain-sensitive structures. The pain stays in your lower back.
Characteristics include:
- Pain centered in the lower back at the specific disc level
- Worsening with sitting and forward bending due to increased intradiscal pressure
- Muscle spasms often accompany the pain as a protective response
Relief with position changes that reduce disc loading
2. Radicular Pain (Leg Pain from Nerve Irritation)
Radicular pain is pain that radiates from your spine down your leg, along a specific nerve distribution. This occurs when herniated disc material compresses or irritates a nerve root.
Important: Radicular pain indicates nerve compression, but the nerve compression doesn't cause your back pain. If you have both back pain and leg pain, you have two separate problems:
- Disc injury causing axial back pain
- Nerve compression causing radicular leg pain
3. Neurogenic Claudication (Leg Pain from Spinal Stenosis)
Neurogenic claudication is leg pain, heaviness, or weakness that occurs with walking and improves with rest. This type of leg pain happens when spinal stenosis compresses nerves during upright activity.
Critical point: Neurogenic claudication from stenosis causes leg symptoms. If you have stenosis and back pain, the back pain has a different source, usually disc injury or facet arthritis. The stenosis and the back pain are separate conditions requiring different evaluation and treatment approaches.
The Average Patient Has Multiple Pain Generators
Most chronic back pain patients don't have a single pain source. They have multiple structural problems generating pain simultaneously. In my clinical experience, patients often have disc injuries at multiple levels (such as L4-L5 and L5-S1), facet arthritis at those same levels, and sacroiliac joint dysfunction, all contributing to overall pain.
This multi-source reality explains why some patients improve 50-60% after surgery targeting only one structure but still have residual pain. The surgery successfully treated one or two pain generators, but other sources remain active and continue generating symptoms.
Comprehensive diagnosis identifies all significant pain generators before treatment planning begins.
Why Most Doctors Struggle With Back Pain Diagnosis
Most physicians cannot accurately diagnose the source of back pain using standard evaluation methods. This isn't a reflection on individual competence. This is a structural problem with how medical training approaches spine pain.
Doctors are trained to identify abnormalities on imaging. They look at your MRI, see a herniated disc or spinal stenosis, and assume that's your pain source. But research published in the New England Journal of Medicine by Jensen et al. (1994) shows that up to 64% of asymptomatic adults have disc abnormalities visible on MRI. Studies of people over age 45 show even higher rates. Disc herniations, bulges, and degenerative changes appear in nearly everyone.
Only 10-15% of visible disc abnormalities actually cause symptoms. The rest are incidental findings. These are abnormalities that look dramatic on imaging but aren't generating any pain.
Proper diagnosis requires correlating three elements:
- Pain history and pattern: when pain occurs, what makes it better or worse, how it started
- Physical examination findings: specific movements and positions that reproduce or relieve pain
- Imaging correlation: matching MRI findings to the clinical presentation
Most physicians evaluate these elements separately or skip the comprehensive physical examination entirely, relying primarily on imaging interpretation.
The Deuk Spine Exam® combines all three elements systematically to achieve 99% diagnostic accuracy, identifying the actual pain generator rather than just visible imaging findings.
Facet Joint Pain: The Second Most Common Cause
Get MRI and specialist evaluation if:
- Pain persists beyond 6-8 weeks despite conservative treatment
- Neurological symptoms develop: Leg weakness, numbness, tingling, or foot drop
- Bowel or bladder dysfunction occurs: A surgical emergency requiring immediate evaluation
- Pain progressively worsens despite treatment
- Night pain disrupts sleep regularly
- Previous treatments provided only temporary relief
- Pain limits work or daily activities for weeks
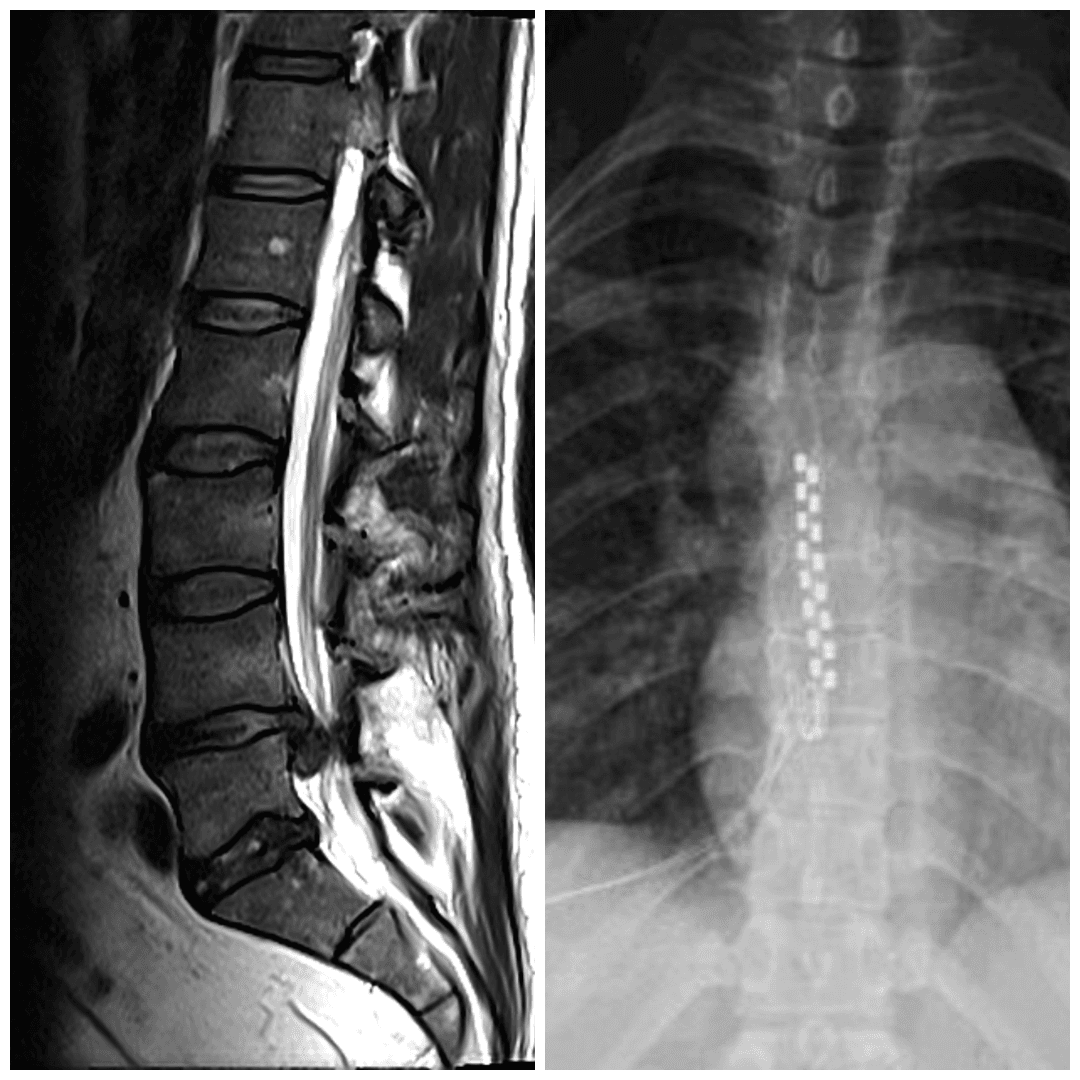
MRI is the diagnostic tool of choice for identifying disc injuries, providing soft-tissue detail that X-rays and CT scans cannot match. Utilize high-field 1.5T or 3T MRI to ensure optimal resolution and diagnostic clarity.
An MRI clearly visualizes:
- Disc herniations and their size/location
- Annular tears (high-intensity zones on T2-weighted images)
- Nerve root compression
- Spinal stenosis
- Facet joint arthritis
- Other structural abnormalities
But MRI shows anatomy, not pain. Connecting imaging findings to your symptoms requires clinical expertise. This is why the Deuk Spine Exam® combines MRI findings with pain history and physical examination, to determine which abnormalities on imaging are actually causing your pain versus which are incidental findings.
Sacroiliac Joint and Piriformis Pain
You've probably heard that poor posture, weak core muscles, tight hamstrings, or being overweight cause back pain. These explanations are convenient because they suggest simple solutions. But if lifestyle factors caused chronic back pain, everyone with poor posture would have chronic pain. They don't.
Here's what actually happens: You have a disc injury: an annular tear with disc disruption, causing inflammation. That disc injury makes certain positions painful, so you naturally adjust your posture to avoid pain. Your back muscles spasm in response to the disc injury, creating "poor posture" as a symptom of the underlying problem.
Weak core muscles don't cause disc tears and inflammation. Disc tears and inflammation trigger compensatory changes as your body protects the injured area, including reduced activity, which can lead to deconditioning.
This distinction matters because addressing lifestyle factors while ignoring structural problems wastes time and delays proper treatment. Conservative care, including physical therapy, can help some patients when structural damage is minimal, but when significant disc tears, facet arthritis, or other structural problems exist, strengthening alone won't resolve the underlying pathology.
Sacroiliac Joint Pain
The SI joint connects your pelvis to your spine. Inflammation or arthritis in this joint causes pain in the lower back, buttocks, and sometimes down the leg, often mimicking sciatica.
SI joint pain comes from inflammation within the joint space or from ligamentous injury around the joint. The pain pattern typically includes:
- Lower back and buttock pain on the affected side
- Pain with transitions: sitting to standing, getting out of cars
- Pain with prolonged sitting or standing
- Sometimes radiation into the posterior thigh
Permanent treatment requires destroying the pain nerves that supply the SI joint using the Deuk Plasma Rhizotomy® technique.
Piriformis Muscle Pain
The piriformis muscle runs from your sacrum to your hip. Injury from bending and twisting can tear this muscle, creating scar tissue and chronic inflammation within the muscle belly.
The piriformis muscle will not heal completely on its own once chronic inflammation and scar tissue develop. Conservative treatment provides only temporary relief.
The Deuk Piriformis Release® is a minimally invasive outpatient procedure performed through a 4mm incision that permanently eliminates piriformis pain by releasing the scar tissue and inflammatory tissue within the muscle.
When to Seek MRI and Specialist Evaluation
Facet joints are small, weight-bearing joints located behind your discs. Each vertebral segment has two facet joints: one on the left and one on the right.
Facet joint pain develops when the joint capsule tears from injury or when arthritis develops within the joint, creating inflammation similar to disc injury. Capsular tears or arthritic changes trigger inflammatory responses within the joint space.
Characteristics of facet joint pain include:
- Pain worsens with extension (bending backward) as this loads the facet joints
- Relief with flexion (bending forward), which unloads the facets
- Often one-sided initially before progressing to bilateral involvement
- Point tenderness over the affected facet joint
Facet joint pain most commonly occurs at the same levels as disc pain: L4-L5, L5-S1, L3-L4, and L2-L3.
A treatment that permanently eliminates facet pain is destroying the pain nerves that supply the joint. The Deuk Plasma Rhizotomy® uses plasma energy to permanently ablate these medial branch nerves through a 30-minute outpatient procedure.

Why "Lifestyle Causes" Don't Explain Chronic Pain
Accurate diagnosis of pain sources determines treatment success or failure. Different structures require different treatments:
Disc injury with annular tear: Treatment must address the inflammatory tissue around the tear and remove any herniated material compressing the nerve. The Deuk Laser Disc Repair® is a proprietary procedure that removes inflammatory tissue, performs an annular debridement, and allows the disc to heal naturally. In our clinical experience with over 2,700 Deuk Laser Disc Repair® procedures, patients report an average of 99% pain relief for treated pain sources, with a complication rate of only 0.01%.
Facet joint pain: Treatment requires destroying the pain nerves that supply the joint. The Deuk Plasma Rhizotomy® permanently eliminates pain through a 30-minute outpatient procedure using plasma energy to ablate the medial branch nerves.
Sacroiliac joint pain: Also requires destroying pain nerves that supply the joint using the Deuk Plasma Rhizotomy® technique adapted for SI joint anatomy.
Piriformis muscle pain: Treatment requires releasing scar tissue and inflammatory tissue within the muscle through the Deuk Piriformis Release®, a minimally invasive procedure performed through a 4mm incision.
Multiple pain generators: Treatment must address all significant sources. When a patient has multiple pain generators, but treatment addresses only one or two, residual pain persists from the untreated sources.
This is why proper diagnosis before treatment is critical. Treatment must match the specific structural source.
The Inflammation Connection
Acute inflammation is the body's initial response to minor injuries. By deploying inflammatory cells to rebuild damaged tissue, the body lays a foundation for recovery that typically resolves within a 2-week timeframe for soft-tissue repair.
Chronic inflammation from structural problems (annular tears, facet capsule tears, joint arthritis) doesn't resolve on its own. An annular tear in a disc can remain as a structural defect. When disc material and inflammatory tissue persist in and around the tear, ongoing inflammatory responses continue.
Small pain nerve fibers can grow into chronically inflamed tissue through a process called neoinnervation. This innervation by pain nerves can increase pain sensitivity over time. This is why disc pain often worsens gradually over months or years despite conservative treatment.
Addressing chronic inflammation requires treating the structural source. Anti-inflammatory medications provide temporary relief but don't eliminate the underlying structural problem. Long-term improvement requires treating the structures that generate inflammation, removing inflammatory tissue from disc tears, destroying pain nerves in arthritic joints, or releasing chronically inflamed muscle tissue.
Treatment Implications: Why Source Identification Matters
Conservative treatment (physical therapy, medications, injections) succeeds for acute injuries and can help some patients with minor structural problems. However, it fails for most chronic back pain when significant structural damage exists because it doesn't address the underlying pathology.
Physical therapy cannot remove the inflammatory tissue associated with annular tears. Strengthening exercises don't address the structural defects in damaged discs. Core stabilization doesn't eliminate inflammation in arthritic facet joints or resolve chronic muscle inflammation, leading to scar tissue formation.
When structural problems such as significant annular tears, facet arthritis, or chronic muscle inflammation are present, conservative treatment provides only temporary symptom management at best. Symptoms return once treatment stops because the structural source remains untreated.
When symptoms persist beyond 6-12 weeks despite appropriate conservative treatment, continuing the same approach for additional months or years delays definitive treatment and prolongs unnecessary suffering.
Why Conservative Treatment Often Fails for Structural Problems
"Nonspecific Back Pain":
This diagnosis means "we don't know what's causing your pain." There's no such thing as truly nonspecific back pain. Every case has specific structural sources. The diagnosis is nonspecific only because the evaluation was incomplete or the diagnostic tools used were insufficient.
"Muscle Strain":
True muscle strains heal within days to two weeks. If your "muscle strain" persists for months, it's likely a muscle spasm secondary to underlying disc or joint injury, or it may represent a chronic muscle injury with scar tissue formation, requiring different treatment.
"Degenerative Disc Disease":
Degeneration describes MRI findings but doesn't necessarily cause pain. Pain attributed to "degenerative disc disease" actually comes from inflammatory tissue in annular tears within the degenerated disc. Treatment must address the inflammatory tissue and structural defects, rather than merely acknowledging that degeneration exists.
Common Misdiagnoses to Be Aware Of
Getting an accurate diagnosis requires finding a specialist who can correctly identify pain generators through a comprehensive evaluation:
- Seek a spine specialist who focuses exclusively on spine conditions
- Look for comprehensive diagnostic systems like the Deuk Spine Exam® that correlate imaging with clinical findings
- Verify they can treat all major pain generators (disc, facet, SI joint, piriformis)
- Demand specificity: Which specific disc? Which structure within that disc? How do you know?
Accurate diagnosis is the foundation of successful treatment. Treatment based on incomplete diagnosis or imaging findings alone creates unpredictable outcomes.
Getting an Accurate Diagnosis: What You Need
If you've suffered chronic back pain for more than two weeks despite conservative treatment:
- Get MRI imaging: Utilize high-field 1.5T or 3T MRI to ensure optimal resolution and diagnostic clarity
- Seek specialist evaluation with a comprehensive diagnostic assessment like the Deuk Spine Exam®
- Demand specific diagnosis: Which structure is causing pain? How do you know? What's the evidence?
- Understand all your pain generators: Patients often have multiple sources that may need treatment
- Choose treatment matching your diagnosis: Different structures need different treatments
Your chronic back pain has specific structural sources. Poor posture didn't cause it. Weak muscles didn't create it. Lifestyle factors don't fully explain it. Damaged discs, inflamed joints, or injured muscles generate your pain signals. Identifying and treating these specific sources transforms temporary symptom management into long-term improvement.
For a free MRI review to identify your specific pain generators, contact Deuk Spine Institute. We'll evaluate your imaging with the Deuk Spine Exam®, identify all contributing structures, and provide a clear explanation of what's actually causing your pain, not just what we see on your MRI.
Taking Action With Deuk Spine Institute
If you've suffered chronic back pain for more than two weeks despite conservative treatment:
- Get MRI imaging: Utilize high-field 1.5T or 3T MRI to ensure optimal resolution and diagnostic clarity
- Seek specialist evaluation with a comprehensive diagnostic assessment like the Deuk Spine Exam®
- Demand specific diagnosis: Which structure is causing pain? How do you know? What's the evidence?
- Understand all your pain generators: Patients often have multiple sources that may need treatment
- Choose treatment matching your diagnosis: Different structures need different treatments
Your chronic back pain has specific structural sources. Poor posture didn't cause it. Weak muscles didn't create it. Lifestyle factors don't fully explain it. Damaged discs, inflamed joints, or injured muscles generate your pain signals. Identifying and treating these specific sources transforms temporary symptom management into long-term improvement.
For a free MRI review to identify your specific pain generators, contact Deuk Spine Institute. We'll evaluate your imaging with the Deuk Spine Exam®, identify all contributing structures, and provide a clear explanation of what's actually causing your pain, not just what we see on your MRI.
