THE DIFFERENT SURGERIES FOR TWO TYPES OF HERNIATED DISC CONDITIONS
A herniated disc is quite common and can cause significant pain, numbness, or weakness in an arm or a leg, depending on the location of the disc in the spine. A spine specialist will conduct a comprehensive evaluation to identify the best course of action. In almost all cases, surgery is only considered after a patient has failed to find relief from medication and pain injections. It's essential to note that these include physical therapy, chiropractic care, pain medication, and pain injections. It's important to note that the patient experiences neck pain or back pain, as well as the type of herniated disc
HERNIATED DISCS: INSTABILITY VS. INSTABILITY
Herniated Disc Without Instability
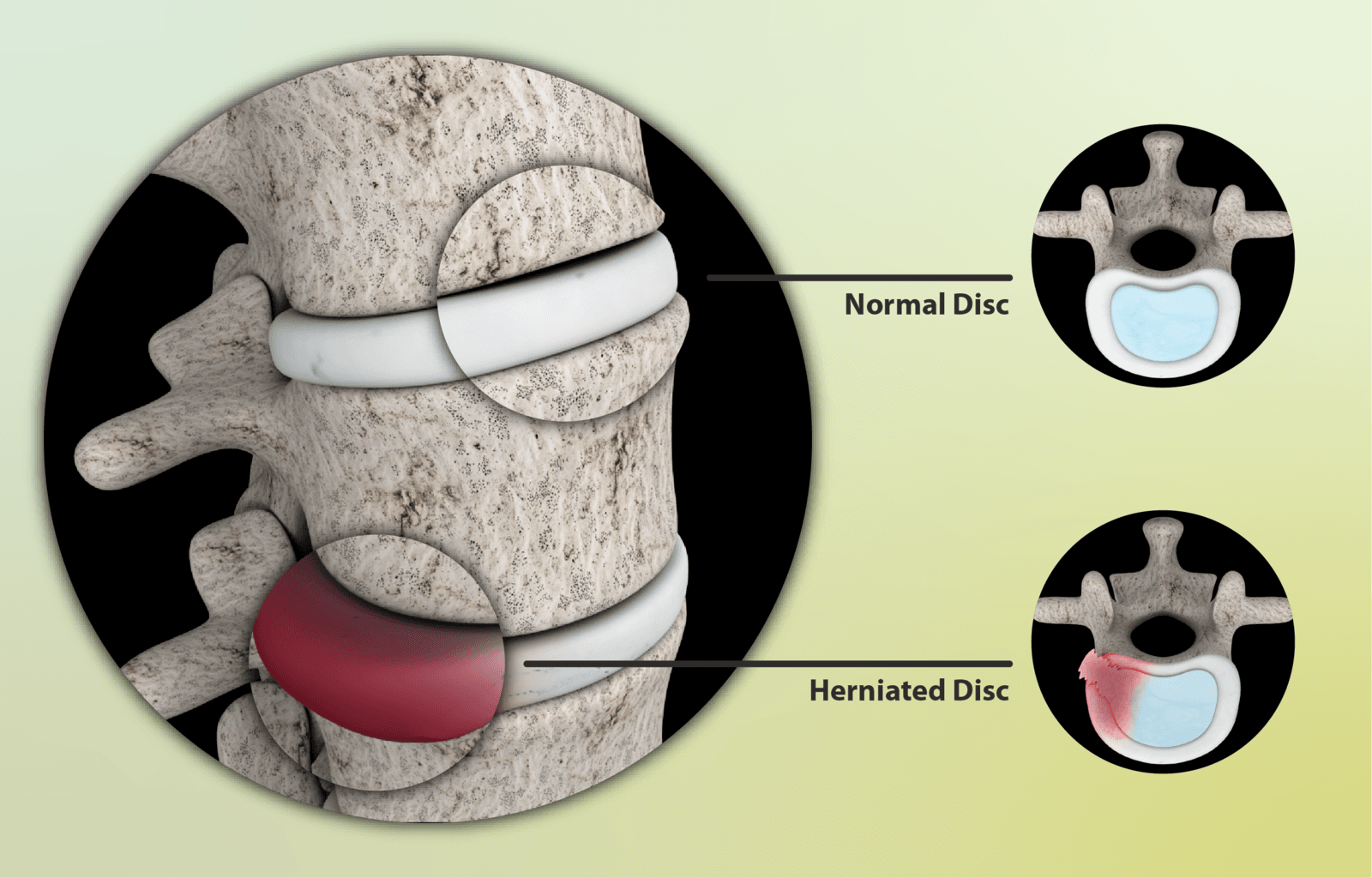
This common type of herniated disc occurs when a piece of the disc's inner material (nucleus pulposus) breaks through the outer layer and presses against a nerve. This nerve compression leads to symptoms such as radiating pain, numbness, or weakness (like sciatica). The aim of surgery is to decompress the nerve by removing the herniated disc fragment.
The typical surgical options for this include:
- Microdiscectomy is a minimally invasive procedure where a small incision is made, and a surgeon uses a microscope to carefully remove only the part of the disc causing the problem. This approach minimizes damage to surrounding muscles and tissue. Usually, the procedure leads to quicker recovery, less post-operative pain, and a high success rate in relieving leg pain (sciatica). It is often done as an outpatient procedure.
- Foraminotomy or laminotomy are surgical procedures aimed at creating more space and reducing pressure on the spinal nerves. Sometimes, a surgeon may perform these procedures along with a discectomy or as standalone treatments if herniation is not the main cause of nerve compression. A foraminotomy widens the bony opening (foramen) through which the nerve root exits the spinal canal, helping to relieve pressure if a disc or bone spur compresses it. A laminotomy involves removing a small section of the lamina (the bony arch at the back of the vertebra) to increase space for the nerve root and give the surgeon access to the herniated disc.
- Discectomy (Endoscopic Spine Surgery) is a advanced, minimally invasive procedure that uses a small camera (endoscope) to reach the herniated disc through a tiny incision (less than one inch wide). The surgeon inserts the endoscope and specialized tools through this small opening to see and remove the herniated disc material. This method avoids cutting muscles and uses a continuous flow of water to enhance visualization and reduce blood loss.
- Laminectomy is a surgical procedure that involves removing part or all of the lamina, a bony plate. Cord or spinal nerves. It is a common surgery, especially for older adults, and is often used to treat conditions like spinal stenosis.
Herniated Disc With Instability
Spinal fusion is the primary surgical procedure for a herniated disc with spinal instability. Simply removing the disc fragment (a discectomy) is not enough, as the instability would remain and could lead to ongoing pain or additional surgery. Spinal fusion is a significant operation that permanently fuses two or more vertebrae into a single, solid bone. This stops movement at the unstable segment, which is crucial for relieving pain and preventing further nerve irritation. While a discectomy alone works for a stable herniated disc, it is not enough for an unstable spine. The main issue is the instability itself. By permanently stopping motion at the unstable segment, fusion offers a long-term solution that:
- Relieves nerve compression: It prevents excessive movement that repeatedly pinches and irritates the nerve.
- Provides stability: Restores proper alignment and prevents further slipping or misalignment—movement of the vertebrae.
- Reduces pain: It eliminates the pain caused by the abnormal motion of the vertebrae.
The general process for a spinal fusion for a herniated disc with instability involves three key steps:
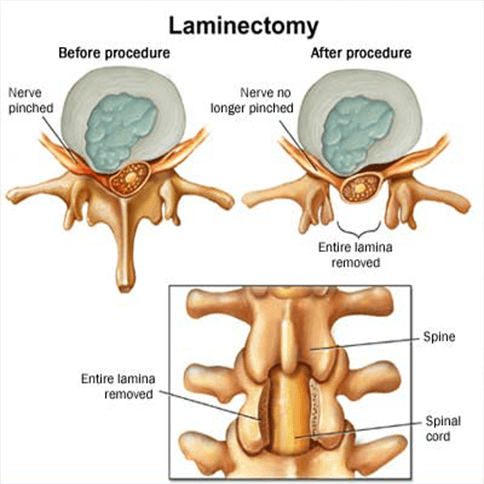
- Decompression: The surgeon first performs a discectomy to remove the herniated disc material pressing on the nerve. To improve access, they may also perform a laminotomy (removing a small part of the bony arch of the vertebra) or a foraminotomy (enlarging the opening where the nerve exits).
- Instrumentation: To securely hold the vertebrae during healing and fusion, surgeons use metal hardware, including screws, plates, and rods. This hardware provides immediate stability and proper alignment.
- Bone Grafting: A bone graft is placed where the disc was removed. This graft can come from the patient's own body (autograft), a donor (allograft), or a synthetic substitute. The purpose of the graft is to act as a scaffold for new bone growth. Over time, the vertebrae will fuse into one solid bone.
There are various types of lumbar spinal fusion procedures, each named according to the specific surgical approach used.
- Anterior Lumbar Interbody Fusion (ALIF): The surgeon approaches the spine from the front (anterior) through an incision in the abdomen. This approach is commonly used for conditions such as degenerative disc disease and spondylolisthesis.
- Lumbar Interbody Fusion (PLIF): This procedure addresses issues in the lower back (lumbar spine). The surgeon approaches the spine from the back, removes the disc, and inserts the bone graft and instruments from that side.
- Transforaminal Lumbar Interbody Fusion (TLIF): This is a variation of the PLIF where the surgeon accesses the disc space through the side (foramen) of the spine, which may be less disruptive to the muscles and nerves.
- Extreme Lateral Interbody Fusion (XLIF): This minimally invasive procedure for the lumbar spine involves making an incision on the patient's side, allowing the surgeon to access the disc from a different angle, which may result in less muscle disruption.
- Oblique Lateral Interbody Fusion (OLIF): This is a minimally invasive spinal fusion procedure that treats various lumbar spine conditions by approaching the spine from the side at an oblique, or angled, trajectory. The approach is designed to be a "sweet spot" between the anterior and lateral approaches, aiming to reduce the risks associated with both.
Artificial Disc Replacement may be considered in rare and specific cases for a disc that has some instability. However, this is usually seen as a less suitable option for significant unrest, as the goal of an artificial disc is to preserve motion. In contrast, genuine instability requires removing motion to be corrected.
THE DEUK DIFFERENCE
Unlike invasive lumbar spinal surgeries, the Deuk Spine Institute performs the least invasive, yet most advanced, spinal procedure in the world – the proprietary Deuk Laser Disc Repair. This procedure is performed without cutting or compromising healthy muscle, fascia, or bone and without the use of risky hardware, resulting in minimal post-operative pain. Best of all, the recovery time is less than three days.
HOW IT’S DONE
We use our proprietary Deuk Laser Disc Repair procedure, a patented, minimally invasive endoscopic laser spine surgery—the only one of its kind worldwide—to treat back and neck pain. An endoscope is inserted through a small skin opening at the affected level, and a laser removes damaged tissue from the annular tear at the back of the disc, eliminating the source of pain. In cases where facet arthritis is also a concern, we utilize our proprietary Deuk Plasma Rhizotomy to alleviate arthritic joint pain.
SEE THE SURGERY LIVE
Our goal is to ensure complete transparency about our process and procedures for fixing back issues, helping our patients and others suffering from debilitating back and neck pain regain their ability to live fully. We livestream our surgeries with our patients' written consent, enabling you to observe our technique.
WHAT TO EXPECT
It takes less than an hour, and our patients leave the outpatient clinic a few hours after surgery feeling no pain and not needing addictive painkillers. They come back the next day for a postoperative review.
OUR SUCCESS RATE
Our success rate is 99.5%, and we have treated thousands of patients who are now living pain-free. It took 20 years and thousands of surgical hours to discover the root cause of chronic back pain and the effectiveness of lasers in treating it.
WE’RE HERE TO HELP
We understand how destructive chronic back pain can be to your life. As neurosurgeons and healthcare professionals, we have committed ourselves to eliminating and curing back pain once and for all. If you’re looking for back pain relief, if you’ve been recommended for a spinal fusion, or are continuing to live with chronic back pain after failed fusion surgery, we can get your quality of life back and help you live pain-free.
OUR COMMITMENT
Your back is one of the most vital parts of your body, consisting of a complex network of nerves, bones, and tissues. That’s why our entire staff is dedicated to providing the highest level of patient care. We hold each other accountable and set high standards for every team member.