Immediate Surgical Complications
These are high-risk events that can occur during or immediately following the surgery:
Spinal cord and nerve root injury:
While rare, direct mechanical trauma or disruption of blood supply can lead to a new or worsened spinal cord injury. Nerve roots near the site may also be damaged, causing pain, numbness, or weakness. Post-operative swelling or the nerves adjusting to their new position can cause temporary irritation, leading to pain, numbness, or tingling. In some cases, nerve damage can be permanent, especially if the nerve was compressed for a long time before the surgery. If nerve roots are already damaged (or become scarred post-surgery), symptoms such as pain, numbness, or weakness may persist despite the fusion.
Excessive bleeding:
Spinal fusion is a surgical procedure that carries a risk of significant blood loss, which can lead to various complications, including anemia. The amount of bleeding can vary depending on the complexity of the surgery, the number of vertebrae being fused, and individual patient factors. Causes of bleeding may include:
- Surgical exposure: The process of exposing the spine and stripping muscle from bone can cause bleeding from exposed muscle and bone surfaces.
- Bone bleeding: Procedures like laminectomy or osteotomy, which involve resecting bone, can cause substantial bleeding from the cancellous bone.
- Epidural bleeding: This is often the most problematic type of bleeding in spine surgery. The epidural venous plexus is a delicate network of veins that surrounds the spinal cord. Damage to these veins can lead to difficult-to-control bleeding, risking nerve damage.
- Large blood vessel injury: A rare but catastrophic event, an injury to a major blood vessel near the spine can cause rapid, life-threatening bleeding.
Spinal fluid leak (CSF leak):
A spinal fluid leak, also known as a cerebrospinal fluid (CSF) leak, is a potential complication of spinal fusion surgery. Cerebrospinal fluid (CSF) is a clear liquid that surrounds and cushions the brain and spinal cord. It is contained within a protective membrane called the dura mater. A CSF leak occurs when a tear or hole in the dura mater allows CSF to escape. Spinal fusion surgery involves working near the spinal cord and its protective coverings. During the procedure, the dura mater can be accidentally torn, leading to a CSF leak. This is a known complication of spine surgery, and while the surgeon will attempt to repair any tear at the time of the operation, a leak can still develop afterward.
General systemic risks:
As with any major operation, complications such as a heart attack or pneumonia are possible and must be managed during the recovery period.
- Heart attack: The risk of a heart attack during or after spinal fusion surgery is a serious but relatively rare complication. Studies have shown that the incidence of cardiac complications after spine surgery is low, but the consequences, including mortality, can be significant for those who experience them. While the event itself is rare, the 30-day mortality rate for patients who do have a cardiac event after lumbar fusion can be alarmingly high, with one study reporting a rate of 24.6%.
- Pneumonia: Pneumonia is a known risk and potential complication of spinal fusion surgery, and it's a concern that is addressed by medical professionals both before and after the procedure. The stress of surgery and the use of anesthesia can affect a patient's respiratory system. Anesthesia can alter lung volumes, reduce the drive to breathe deeply, and impair muscle function. This can lead to atelectasis (pulmonary collapse), where parts of the lungs don't inflate properly, creating an environment where bacteria can grow. After spinal fusion, patients are often limited in their movement, which can make it challenging to take deep breaths and cough effectively. Pain from the incision can also lead to shallow breathing, further increasing the risk of fluid and secretions building up in the lungs, which can lead to pneumonia.
Post-Operative Failure and Healing Issues
These complications can affect the success and longevity of the surgery:
Failed fusion (pseudarthrosis):
This is a significant cause of pain. It occurs when the bones don't successfully fuse as intended. The bones don’t fuse completely, meaning the motion persists—causing ongoing discomfort and instability. This happens in up to 5-20% of cases, especially if the patient smokes, there’s poor bone quality (e.g., osteoporosis), or if the hardware loosens or breaks.
Discover How One Patient Overcame Multiple Failed Fusion Surgeries with DLDR®
Hardware failure:
The screws, rods, or plates used to stabilize the spine during the fusion process can sometimes loosen, break, or irritate surrounding tissues, causing pain, and may need to be removed. This can lead to symptoms like persistent or worsening back pain, muscle spasms, and a feeling of instability. In some cases, patients may even feel a bulge or a scraping/grinding sensation (crepitus) near the surgical site. Even if the hardware is securely in place, it can still cause pain. Misplaced hardware can irritate or press on nearby nerves, leading to symptoms such as sharp, burning pain, tingling, or numbness in the back, arms, or legs. Sometimes, hardware can also be prominent under the skin, causing discomfort and a painful bump. In rare cases, a patient may be sensitive to or have an allergic reaction to the metal used in the hardware, which can cause it to loosen. Just the nature of drilling and seating metal hardware into healthy bone can cause permanent muscle damage, injury to internal organs, permanent muscle damage, permanent disability, or even death.
Spinal infection:
Although rare, an infection at the surgical site can cause pain, swelling, warmth, and a fever. Infections can occur due to a longer surgical duration, the use of hardware, or more extensive or complex procedures. The incidence of surgical site infections (SSIs) after spine surgery varies, with reported rates ranging up to 18.8%, depending on procedure complexity and patient risk factors.
Scar tissue formation (epidural fibrosis):
While scar tissue is a regular part of the healing process, a buildup of scar tissue around a nerve root can put pressure on the nerve and cause pain. While scar tissue itself doesn't have nerve endings and typically doesn't cause pain, it can become a source of discomfort if it forms excessively around a nerve root, leading to compression, inflammation, or irritation. This is a common cause of "failed back surgery syndrome" (FBSS), a condition where patients experience persistent or recurring pain after a spinal procedure.
Find Out if You're a Candidate
Upload your MRI and schedule a free consultation with Dr. Deukmedjian to learn if our minimally invasive treatment can help you get back to a healthy life.

Long-Term Biomechanical Consequences
These issues arise over time as the body compensates for the fused segment:
Adjacent segment disease (ASD):
When vertebrae are fused, the segments above and below the fusion have to compensate for the lost mobility. This can put increased stress on these adjacent segments, leading to accelerated wear and tear and new pain. Fusing one level of the spine can put extra stress on the discs and joints above and below, leading to new pain and prolonged degenerative disc disease. When a segment of the spine is fused, the vertebrae directly above and below have to compensate for this loss of motion, leading to increased stress and strain on nearby segments, causing accelerated degenerative disc disease, which can lead to:
- Spinal stenosis is a narrowing of the spinal canal that puts increased pressure on the spinal cord or nerves.
- Disc herniation, where a disc can rupture, pushing out and irritating nearby nerves.
- Facet joint arthritis, where the small joints that connect the vertebrae can become inflamed and arthritic.
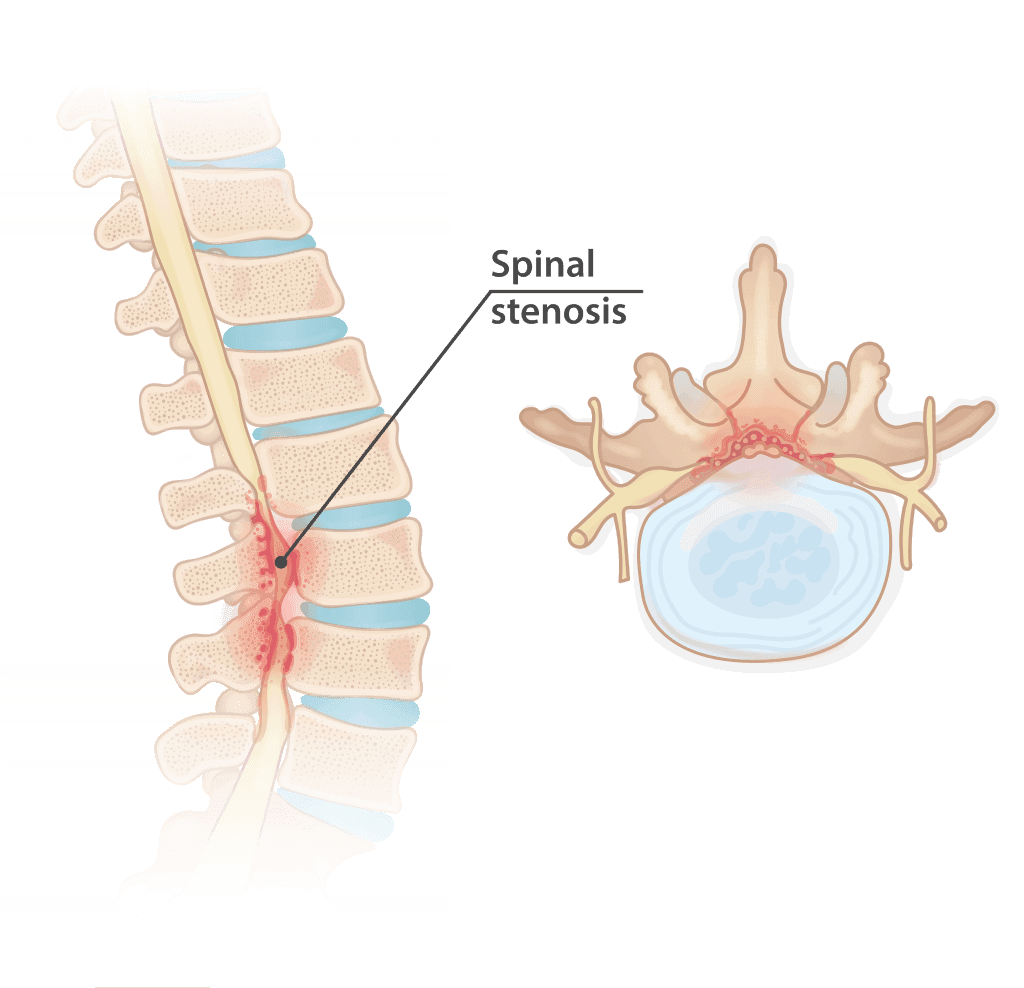
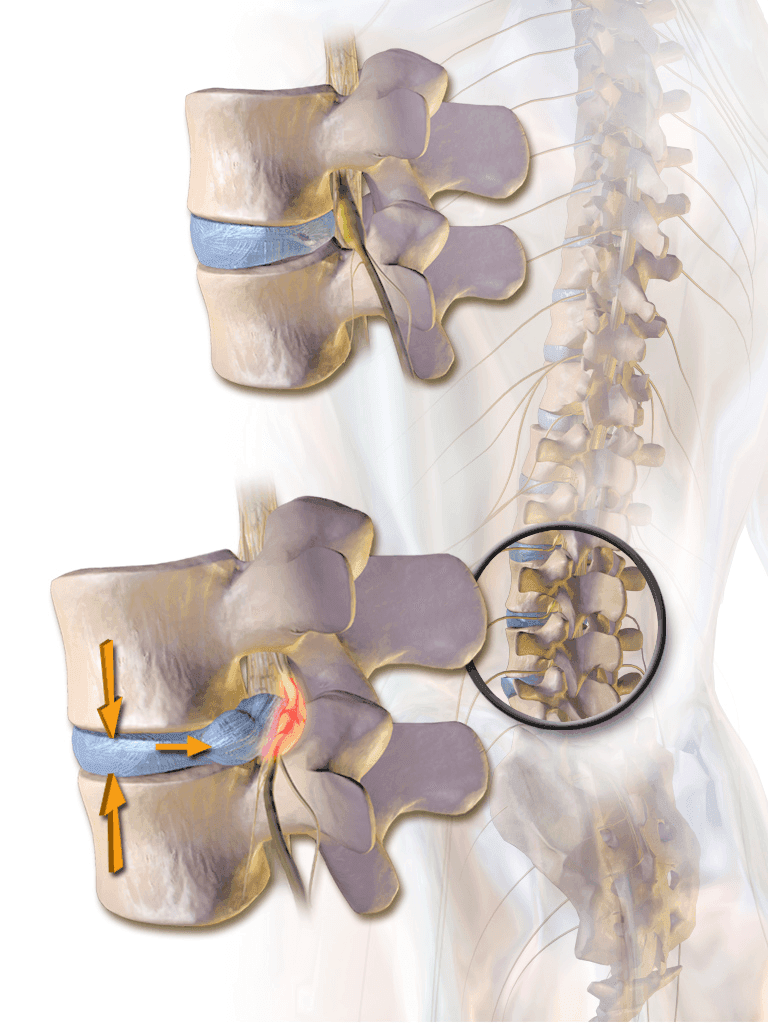
Images: Herniated disc and spinal stenosis. Pain from a herniated disc may subside for a few months, but ultimately will become chronic because the disc cannot heal itself. Spinal stenosis must be treated with surgery to alleviate the symptoms. Injections, pain medicines, and therapy do not work in the long term for either condition.
Muscle injury and atrophy:
Also known as muscle atrophy or fatty degeneration, muscle death occurs due to the surgical cutting involved and is a key source of post-surgical pain. That is due to loss of support, chronic inflammation, scar tissue, and tight fascia around atrophied muscles. Recovery takes months, and the pain doesn’t always necessarily subside. Additionally, fusion surgery can damage muscle in other ways: Paraspinal muscles may be cut, retracted for prolonged periods, or have their nerve supply damaged. This can lead to loss of movement at one or more vertebrae, resulting in the muscle having less work to do and weakening quickly. Additionally, chronic disuse after surgery can reduce muscle activation, leading to atrophy over time.
Flat back syndrome:
A condition that can occur after spinal fusion surgery, particularly in the lumbar (lower) spine. Usually, the spine has natural curves: an inward curve in the neck (cervical lordosis), an outward curve in the middle back (thoracic kyphosis), and another inward curve in the lower back (lumbar lordosis). These curves work together to keep the body's center of gravity aligned over the hips and pelvis, allowing a person to stand upright with minimal muscle effort. So, Flat Back Syndrome is a type of "sagittal imbalance," which means there's an imbalance in the front-to-back alignment of the spine. If the spine heals in an abnormal position, it can lead to poor posture, long-term discomfort, and progressive back pain.
Sacroiliac (SI) joint pain:
The SI joint , located at the base of the spine, can experience increased stress after spinal fusion, leading to pain. The primary reason for SI joint pain after spinal fusion is a change in the way forces are distributed throughout the lower back and pelvis. When vertebrae are fused, the mobility of that segment of the spine is eliminated. This causes the adjacent joints, including the SI joint, to compensate for the lost motion. The SI joint, which usually has minimal movement, may be subjected to increased stress and strain, leading to several potential problems. Research has shown a significant percentage of patients with persistent back pain after spinal fusion have SI joint pain, with some studies reporting the incidence to be between 16 and 32 percent.
The Deuk Difference: A Minimally Invasive Alternative
If you are facing the high risks associated with spinal fusion, there is an alternative. The Deuk Spine Institute offers a procedure designed to provide lasting relief without compromising your long-term spinal health.
Spinal fusion surgery is an invasive procedure that requires cutting into healthy muscle fibers to fuse vertebrae with metal hardware, presenting many surgical risks.
Learn How Deuk Laser Disc Repair® Works
Watch this short explainer video to understand how our minimally invasive surgery can help you live pain-free.
Deuk Laser Disc Repair®
We treat chronic back and neck pain with a patented, minimally invasive endoscopic laser spine surgery—the only one of its kind in the world.
- No fusion: We perform no bone cutting and insert no metal hardware.
- Targeted repair: A laser is used through a 4mm opening to repair the disc tear and block the nerves that are the root cause of the pain.
- Fast recovery: The procedure takes less than an hour. Patients walk out pain-free within a few hours and are typically cleared to resume a normal life in under three days.
- Proven success: Our procedure boasts a 95% success rate for curing back pain.
We're Here to Help
Take the first step to a pain-free life: upload your most recent MRI for a free review and consultation with the physician who developed the Deuk Laser Disc Repair® procedure.
FAQs
Q: What is the most common long-term complication after spinal fusion surgery?
A: The most common long-term complication is adjacent segment disease (ASD). When vertebrae are fused, the vertebrae directly above and below the fusion must compensate for the loss of mobility. This increased stress causes accelerated wear and tear, leading to new problems in the neighboring segments, such as disc herniation or spinal stenosis, sometimes years after the initial surgery.
Q: How is the Deuk Laser Disc Repair® fundamentally different from a traditional spinal fusion?
A: Traditional spinal fusion is an invasive procedure that involves cutting bone and implanting metal hardware to force vertebrae to grow together. Deuk Laser Disc Repair® is a minimally invasive endoscopic procedure that uses a laser to repair the disc and eliminate the source of pain. It is designed to achieve relief without cutting healthy bone, inserting hardware, or compromising the overall structure and mobility of the spine.
Q: Does pain after a spinal fusion mean the surgery failed?
A: Not necessarily, but persistent pain is a known complication, often termed "failed back surgery syndrome" (FBSS). This can be caused by several factors described in the article, including:
- Failed fusion (pseudarthrosis): The bones did not successfully fuse.
- Scar tissue formation (epidural fibrosis): Excessive scar tissue around a nerve root can cause compression.
- Hardware failure: Screws, rods, or plates have broken or shifted.