Collapsed Disc
A collapsed disc is one of the conditions that can affect the intervertebral disc located in the spinal column. It is often treated as a synonymous syndrome to degenerative disc disease because both illnesses display similar external characteristics.
What is collapsed disc?
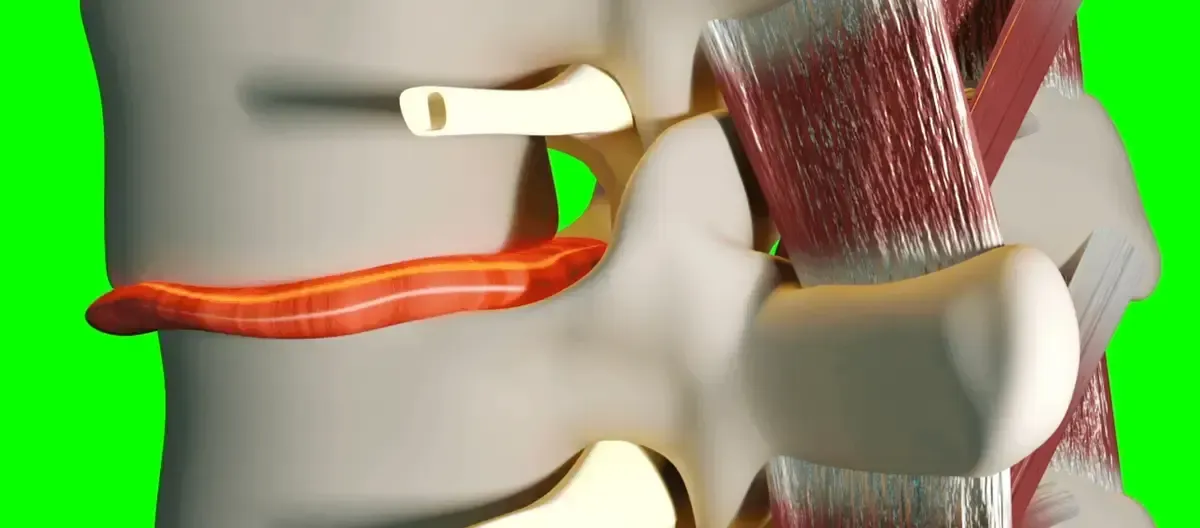
A collapsed disc may occur when intervertebral discs of the spine suffer a loss of overall disc height from degeneration through aging or injury. Discs act as natural shock absorbers in the spine, so when they are damaged, it can cause pain. Weakened or torn annulus fibrosus can cause discs to bulge or become herniated. This causes the disc to lose its normal height and “collapse.” Both of these conditions may cause pressure upon adjacent nerve roots. This can cause symptoms including numbness, tingling, weakness or pain.
Causes of a collapsed disc
A collapsed disc is often the result of Degenerative Disc Disease. Degenerative disc disease involves a variety of structural, biochemical, nutritional and molecular changes that occur in the spinal disc over time or following an initial injury to the intervertebral spinal disc in your spine. Degenerative disc disease is a common cause of back pain and neck pain (discogenic pain), sciatica and radiculopathy. The pain in your back from degenerative disc disease comes from irritated (inflamed or compressed) nerve fibers nearby, and can be categorized as a mechanical instability.
Collapsed discs are more common in those who work in jobs that put a lot of strain on the neck and lower back or that demand a lot of heavy lifting. Excessively obese people may develop this ailment as a result of the additional pressure imposed on the spine. Many people begin to feel the impact of degenerative disc degeneration around the age of forty. The patient is asymptomatic in most cases, but some people may experience intermittent acute pain that might progress to chronic osteoarthritis pain.
How disc degeneration occurs in the spine
When a disc’s cartilaginous endplate is damaged, the blood flow to the discs is disrupted. As a result, there is a loss of nutrients and oxygen, which are required to maintain and repair damaged tissues in the spine. Due to this deficiency, a disc can begin to wear down quite fast once one stress or injury occurs, a process known as the degenerative cascade.
The degenerative cascade is a gradual process that can last 10 to 30 years. In some cases, there is no initial injury that marks the onset of symptoms. However, when it happens, the occurrence of the initial stress often causes acute pain. Following this, stiffness and limited mobility in the back begin to set in. The injured spinal segment is thus subjected to a prolonged period of relative instability. As the disc height declines, the muscles, ligaments, and facet joints around the disc area gradually adjust to reestablish spine stability. There are intermittent flare-ups of moderate to severe low back pain during this phase. Pain and other symptoms usually subside once the spinal section has stabilized.
Symptoms of collapsed disc
Disc degeneration is a normal part of aging, but not everyone experiences pain or other noticeable signs. Symptoms usually appear when there is spinal instability, muscle spasms, and potentially nerve root irritation.
Symptoms of collapsed disc develop based on the location of the disc in the spine:
Lumbar collapsed disc symptoms
A lumbar collapsed disc will often cause symptoms such as pain in your lower back and numbness along the hips, thighs, and legs. The low back pain associated with lumbar degenerative disc disease is usually generated from inflammation of the nerve root when the proteins in the herniated disc tissue irritate the surrounding nerves. The small nerve within the disc space and potentially the larger sciatic nerve that goes down into the legs can be affected.
Micro-motion instability can also cause lumbar pain when the surrounding tissue of the disc, called the annulus fibrosus, becomes worn down and can no longer absorb stress on the spine. The resulting movement along the vertebral segment causes the bones to rub against each other and generate friction.
Cervical Collapsed disc symptoms
When a disc in the cervical spine collapses, patients will experience persistent pain in the neck, which will be worsened by certain motions such as turning and bending the head. This pain can also radiate into the arms and shoulders.
Coupled with the pain, certain sensory functions will be lost or weakened depending on the exact location of the affected disc. Potentially affected areas include the fingers, biceps, and shoulders, where patients experience weakness or complete numbness.
Diagnosis of collapsed disc
X-rays are frequently the first choice since they effectively rule out infection, malignancies, fractures, and congenital disabilities. Myelograms can be performed to evaluate the condition of the spinal cord and nerve roots. However, the best imaging test for identifying inconsistencies in the spine is an MRI.
Identifying a collapsed disc is relatively easy with the use of an MRI. On an MRI, collapsed discs appear to have been crushed or broken. A collapsed disc is often relatively synonymous with degenerative disc disease and shows similar characteristics, such as a darkening of the disc interior and shrinking of the overall disc space. In less common cases, it can be caused by injury.
Because degenerative disc disease is a naturally occurring part of aging, it may not cause symptoms in some patients. To see if a collapsed disc is the cause of pain, a physical exam will need to be performed along with a possible discogram to determine the disc’s integrity. A physical examination assesses the spine’s range of motion and strength. It may include feeling along the spine with the hand to detect soreness, inflammation, or physical anomalies. Furthermore, movement tests that show whether motions or positions relieve or increase pain can aid in determining where the pain originates in the spine.
In addition to the required tests, most physicians will also compile a medical history report. This report will include information about current symptoms, such as when the pain began, whether the pain is accompanied by other symptoms such as numbness or tingling, and whether the pain developed as a result of an injury. Medical history also collects data on frequent physical activity, sleep habits, and previous injuries.
Treatment of collapsed discs
Treatment for a collapsed disc depends on the duration and severity of discogenic pain. If the pain’s duration is less than two months, it may respond well to pain medication, physical therapy, and injections. Discogenic pain lasting longer than two months usually requires a safe, outpatient surgery to relieve painful symptoms effectively.
Deuk Laser Spine Surgery
Deuk Laser Disc Repair is the most advanced laser spine surgery in the world. It is used as an alternative to dangerous invasive surgeries like total disc replacement and spinal fusion.
This revolutionary procedure was developed by Dr. Ara Deukmedjian, a renowned neuro-spine surgeon and a true pioneer in minimally invasive, laser, and endoscopic back and neck pain treatment.
Deuk Laser Disc Repair is a form of endoscopic spine surgery performed in a state-of-the-art outpatient surgery center under sedation while the patient relaxes. This procedure does not compromise or weaken the health and integrity of the spine.
In over 15 years of performing this procedure and with over 1,300 patients treated, there has been a 95% success rate with no complications in any patient.
How Deuk Laser Disk Repair Works
To get started, Deuk Laser Disc Repair requires a very small incision, less than a quarter inch long. A cylindrical rod called a dilator is inserted in the small opening to gently spread the muscle to create a small passage and guide through which the surgery is performed endoscopically. The tip of the dilator is advanced into the symptomatic disc through the tear in the annulus where the herniation originates, and a tube called the retractor slides over the dilator and is carefully positioned into the painful disc. The rest of the entire Deuk laser disc repair surgery will occur inside this narrow tube.
To access the spine, an endoscopic camera is inserted into the tubular retractor to allow the surgeon to guide the laser inside each symptomatic disc. This process ensures that bones and surrounding tissues are not damaged, unlike traditional spinal fusions, microdiscectomy, and artificial discs.
The Holmium YAG laser used in the Deuk laser disc repair is manipulated accurately with millimeter precision under endoscopic visualization to remove only painful inflammatory tissue from the disc. The laser is precisely used to remove damaged disc material that is causing the pain.
Once the laser has removed the inflamed painful part of the annular tear and the herniated nucleus pulposus, the endoscope and tubular retractor are removed, leaving less than one-quarter inch incision in the skin, which can be closed with a single stitch and a band-aid.
The total time for the Deuk laser disc repair surgery is one hour, and the patient is in recovery for about 45 to 60 minutes before being released to go home. Hospitalization is not needed and the risks of hospital-based surgery are avoided.
Also, with the Deuk laser disc repair, there’s no loss of normal movement, and the flexibility of the disc and joint is preserved. With endoscopic Deuk laser disc repair there is no fusion, metal implants or biological material added to the spine. The procedure is all-natural allowing your body to heal the herniated or bulging disc itself.
After the surgery, the Deuk laser disc repair patient is back home, enjoying life with a speedy recovery allowing normal activities without pain. Another advantage of Deuk laser disc repair is that no opioids or powerful narcotic painkillers are needed after surgery. Open spine surgeries like microdiscectomy, laminectomy, artificial disc replacement and fusion all cause so much internal trauma that patients are in severe pain after surgery and must take painkillers for weeks after their surgery but not with Deuk laser disc repair.
At Deuk Spine Institute, we specialize in minimally invasive surgical techniques and comprehensive spine treatments to cure back and neck pain. Our world-class physicians are personally invested in the well-being of every patient. Start your treatment with us today by submitting your MRI online for a free remote review to determine your candidacy for surgery. You can also visit one of our locations in person by calling patient services at 321-255-6670.