By Dr. Ara Deukmedjian, MD | Board-Certified Spine Surgeon
Medically Reviewed: December 31, 2024
Last Updated: December 31, 2024
Reading Time: 18 minutes
Facet hypertrophy, or facet joint hypertrophy, occurs when the small joints in your spine enlarge due to degenerative changes, typically from arthritis or wear and tear. These joints help stabilize your spine and guide movement, but when they become enlarged, they can cause back pain, stiffness, and in some cases, compress nearby spinal nerves, leading to radiating pain in the arms or legs.
Recent research from 2024 shows that facet joint problems account for 15% to 41% of cases of chronic low back pain worldwide.1 While facet hypertrophy cannot be reversed, a range of effective treatments can significantly reduce pain and improve quality of life. This comprehensive guide examines the latest evidence-based approaches to managing facet hypertrophy, from conservative care to advanced minimally invasive procedures.
Understanding Facet Hypertrophy
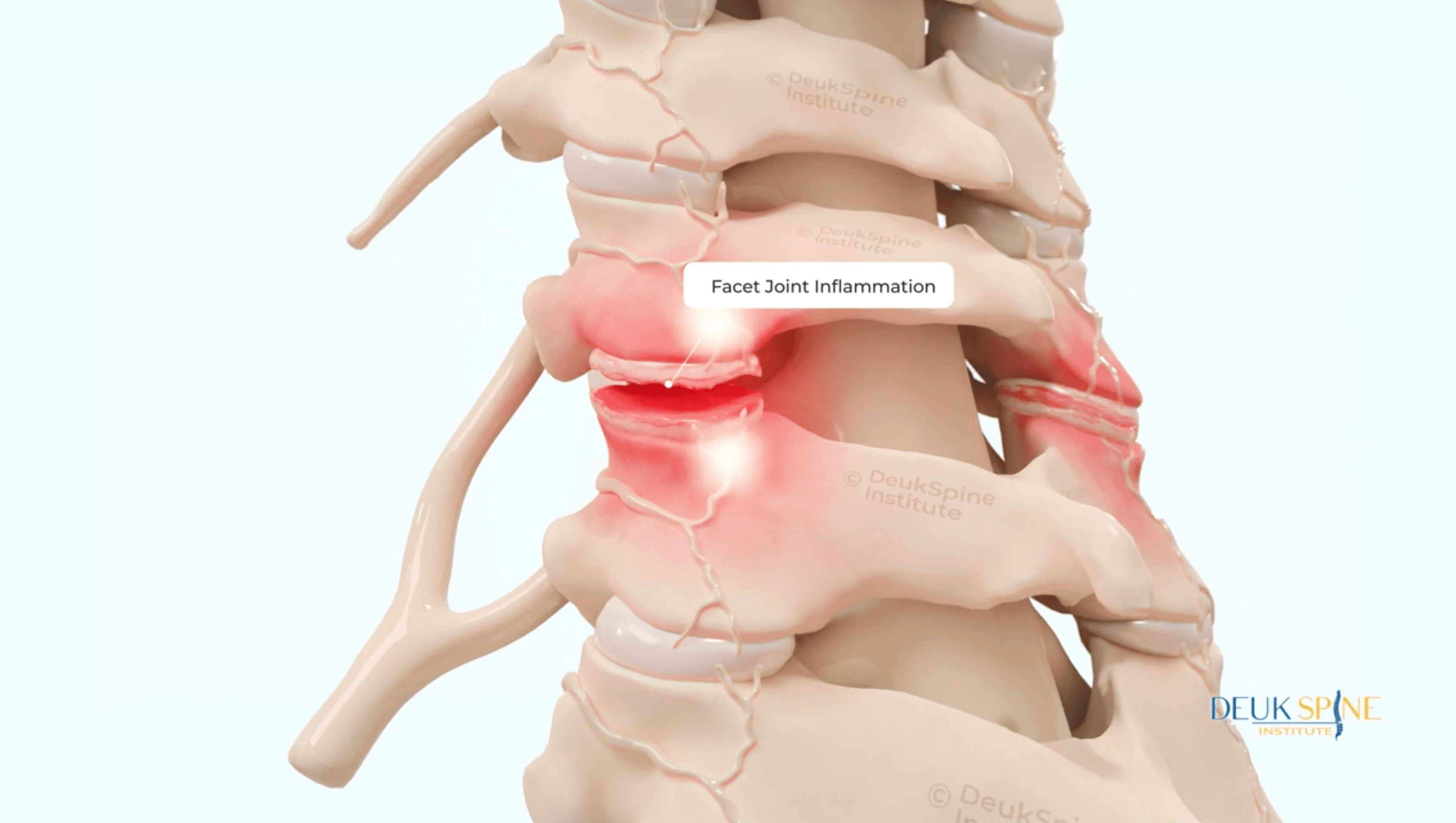
Facet hypertrophy is a condition where the facet joints of the spine become enlarged and inflamed. These are synovial joints located where two vertebrae meet. They play a critical role in stabilizing the spine during bending, twisting, and rotational movements.
What Happens During Facet Hypertrophy
When facet joints undergo degenerative changes, several processes occur:
Cartilage breakdown: The protective cartilage that covers the joint surfaces wears away over time. This cartilage normally distributes pressure evenly across the bone and prevents friction. When it deteriorates, bones begin to rub against each other.
Joint enlargement: As the body attempts to stabilize the degenerating joint, it responds by forming new bone around the joint margins. This is called hypertrophy, which literally means abnormal enlargement.
Inflammation: The joint capsule becomes inflamed in response to ongoing degeneration. The synovium (the lining of the joint) becomes inflamed, and the joint capsule begins to show fibrosis, neovascularization, and eventually extensive fibrocartilage proliferation.2
Osteophyte formation: Bone spurs (osteophytes) commonly form at the edges of the joint, particularly where the joint capsule attaches to bone. These develop as the body’s attempt to stabilize an unstable joint.
Why Location Matters
Facet hypertrophy can occur at any level of the spine:
Cervical facet hypertrophy can affect the neck region and cause neck pain, headaches, and radiating pain into the shoulders and arms.
Thoracic facet hypertrophy occurs in the middle back and is less common but can cause upper back pain and stiffness.
Lumbar facet hypertrophy affects the lower back; the most common location. It often causes lower back pain, stiffness, and, in some cases, leg pain due to nerve compression.
Research from 2024 indicates that facet joint pain comprises 55% of chronic cervical spine pain syndromes, 42% of thoracic spine pain, and 31% of chronic lumbar spine pain.3
Anatomy of the Facet Joints: Why They’re So Important
Structure and Function
Facet joints are small, paired joints located on the back (posterior) side of each vertebra. There are two facet joints at each spinal level, one on the left and one on the right. They are formed by the superior articular process of the lower vertebra articulating with the inferior articular process of the upper vertebra.
These joints serve several critical functions:
Stability: Facet joints help keep your spine stable, preventing excessive movement that could damage the spinal cord or nerves.
Guided movement: The angle and orientation of facet joints determine what types of movements are possible at each spinal level. For example, cervical facet joints allow for more rotation than lumbar facet joints.
Weight distribution: Along with the intervertebral discs, facet joints help distribute the mechanical load placed on the spine. In a healthy spine, approximately 80% of your weight is distributed across the intervertebral disc and 20% the facet joints.3
What Happens When Discs Degenerate
When the intervertebral disc loses height due to degeneration, a significant shift occurs in how weight is distributed across the spine. The facet joints must bear more load than they were designed to handle. This excessive stress accelerates the degenerative process in the facet joints themselves, leading to cartilage breakdown and eventual hypertrophy.
Nerve Supply
Each facet joint receives sensory innervation from two spinal levels: The medial branch nerve at the same vertebral level and the medial branch nerve from one level above. This dual innervation pattern explains why facet-related pain is often difficult to pinpoint precisely and why it can feel diffuse rather than localized.
Common Symptoms of Facet Hypertrophy
Symptoms of facet hypertrophy vary depending on the severity of joint enlargement, the specific spinal level affected, and whether nerve compression is present.
Typical Pain Patterns
Localized back or neck pain: Most patients experience pain directly over the affected facet joints. This pain is typically worse with extension (bending backward) and rotation (twisting) of the spine.
Morning stiffness: Pain and stiffness are often worse after periods of inactivity, particularly first thing in the morning. This pattern is characteristic of arthritic conditions.
Pain with certain movements: Activities that load the facet joints, such as prolonged standing, walking downhill, or arching the back, tend to increase pain.
Relief with forward bending: Many patients find temporary relief by bending forward or sitting, as these positions open up the facet joints and reduce pressure on them.
Referred Pain Patterns
Facet joint pain commonly refers to other areas of the body in predictable patterns:
Cervical facet hypertrophy can cause:
- Headaches, particularly at the base of the skull
- Pain radiating into the shoulders and upper back
- Pain between the shoulder blades
Thoracic facet hypertrophy can cause:
- Pain wrapping around the rib cage
- Pain in the mid-back region
Lumbar facet hypertrophy can cause:
- Pain radiating into the buttocks
- Pain in the hips and groin
- Pain in the upper thighs
It’s important to note that this referred pain follows a non-dermatomal pattern, meaning it doesn’t follow the specific nerve root distributions seen with disc herniations.
Neurological Symptoms
When facet hypertrophy becomes severe enough to compress spinal nerves, additional symptoms may develop:
Radicular pain: Sharp, shooting pain that travels down an arm or leg following a specific nerve root distribution.
Numbness and tingling: Abnormal sensations in the arms, hands, legs, or feet.
Weakness: Difficulty with specific movements, such as lifting the foot (foot drop) or gripping objects.
Neurogenic claudication: In cases of lumbar spinal stenosis caused by facet hypertrophy, patients may experience leg pain, weakness, or numbness that worsens with walking and improves with sitting or bending forward.
Physical Examination Findings
During a physical examination, healthcare providers look for specific signs:
Tenderness: Direct tenderness over the affected facet joints when palpating (pressing on) the spine.
Limited range of motion: Reduced ability to extend (bend backward) or rotate the spine.
Positive Kemp’s test: Pain is reproduced when the examiner assists the patient in extending and rotating the spine toward the painful side.
Muscle spasm: Tightness or spasm in the paraspinal muscles as they attempt to splint and protect the painful joint.
Causes and Risk Factors for Facet Hypertrophy
Facet hypertrophy develops through a combination of natural aging processes and specific risk factors that accelerate joint degeneration
Primary Causes
Degenerative disc disease: The most common cause of facet hypertrophy is age-related disc degeneration. As discs lose height and their ability to absorb shock, excessive stress transfers to the facet joints. Research shows that 89% of people aged 60 to 69 have facet joint osteoarthritis, though not all experience symptoms.4
Osteoarthritis: Like other joints in the body, facet joints can develop osteoarthritis, the “wear and tear” arthritis that commonly affects aging joints. This process involves cytokines and proteolytic enzymes that break down cartilage and stimulate bone remodeling.
Trauma and injury: Sudden injuries from car accidents, sports impacts, or falls can damage facet joints and accelerate the degenerative process. Even minor repetitive trauma from poor posture or repetitive movements can contribute over time.
Spondylolisthesis: This condition involves one vertebra slipping forward on the vertebra below it. This instability places excessive stress on the facet joints, often leading to hypertrophy as the body attempts to stabilize the segment. For more information on spinal instability, see our article on foraminal narrowing.5
Inflammatory Conditions
Certain systemic inflammatory conditions can affect facet joints:
Rheumatoid arthritis: This autoimmune condition can cause inflammation in facet joints, leading to synovitis (inflammation of the joint lining) and subsequent joint damage.
Ankylosing spondylitis: This inflammatory arthritis primarily affects the spine and can lead to inflammation and eventual fusion of facet joints.
Gout: In rare cases, crystal deposits in facet joints can cause acute inflammation and contribute to chronic joint changes.
Risk Factors
Several factors increase the likelihood of developing facet hypertrophy:
Advanced age: The prevalence of facet joint disease increases significantly after age 50.
Previous spine injury: A history of trauma to the spine, even if it occurred years ago, increases risk.
Poor posture: Chronic poor posture places abnormal stress on facet joints and accelerates degeneration.
Obesity: Excess body weight increases the mechanical load on spinal structures, including facet joints.
Occupation: Jobs involving repetitive bending, twisting, or heavy lifting place extra stress on facet joints.
Genetics: Family history of degenerative arthritis may increase susceptibility to facet joint degeneration.
Lack of physical activity: Weak core and back muscles fail to adequately support the spine, placing more stress on passive structures like facet joints.
How Facet Hypertrophy Leads to Spinal Stenosis
One of the most clinically significant consequences of facet hypertrophy is its contribution to spinal stenosis, or narrowing of the spaces within the spine.
Types of Stenosis Caused by Facet Hypertrophy
Central canal stenosis: As facet joints enlarge, they can narrow the central spinal canal where the spinal cord (in the cervical and thoracic regions) or cauda equina (in the lumbar region) resides. For more information, see our guide on spinal canal stenosis.6
Foraminal stenosis: The neural foramina are the openings on either side of the spine where nerve roots exit the spinal canal. Hypertrophied facet joints can narrow these openings, compressing the exiting nerve roots. This is particularly common when the superior articular process becomes enlarged. For detailed information, see our article on foraminal stenosis.
Lateral recess stenosis: This involves narrowing of the space just before the nerve root enters the foramen. Facet hypertrophy is one of the most common causes of lateral recess stenosis.
Additional Contributing Factors
Facet hypertrophy rarely occurs in isolation. Other degenerative changes often accompany it:
Ligamentum flavum hypertrophy: The ligamentum flavum is a ligament that runs along the back of the spinal canal. As facet joints degenerate, this ligament often thickens and bulges into the spinal canal, further narrowing the available space for nerves.
Osteophyte formation: Bone spurs that develop on hypertrophied facet joints can project into the spinal canal or foramina.
Facet joint cysts: Some patients develop synovial cysts arising from degenerated facet joints. These fluid-filled sacs can compress nerve roots. Studies show that about half of these cysts recur even after initial rupture or treatment.7
Clinical Significance
When facet hypertrophy causes significant stenosis, patients may develop:
- Neurogenic claudication (leg pain with walking)
- Radiculopathy (pinched nerve symptoms)
- In severe cervical cases, myelopathy (spinal cord compression)
- Chronic, disabling pain affecting quality of life
Looking for a Second Opinion?
Upload your latest MRI for a free virtual consultation and review with Dr. Ara Deukmedjian, MD.
Accurate Diagnosis of Facet Hypertrophy
Diagnosing facet hypertrophy requires a combination of clinical evaluation and imaging studies. However, diagnosis can be challenging because imaging findings don’t always correlate with symptoms.
The Diagnostic Challenge
One of the most important things to understand about facet hypertrophy is that imaging changes are common in people without pain. Research shows that radiologic evidence of facet joint degeneration can be found in many asymptomatic individuals.4 This means that simply seeing facet hypertrophy on an MRI doesn’t automatically mean it’s the source of your pain.
The key to accurate diagnosis is correlating imaging findings with your specific symptoms and physical examination findings.
Clinical Evaluation
A thorough evaluation begins with:
Medical history: Your healthcare provider will ask about the character, location, and timing of your pain, as well as what makes it better or worse.
Physical examination: This includes palpation of the spine, assessment of range of motion, neurological testing (reflexes, strength, sensation), and provocative tests like Kemp’s test.
Symptom correlation: The physician will determine whether your symptoms match the pattern typically seen with facet joint problems.
Imaging Studies
X-rays: Plain radiographs can show joint-space narrowing, osteophytes, and alignment abnormalities. However, they provide limited information about soft tissues and neural structures.
CT scan (Computed Tomography): CT provides excellent detail of bony structures. It clearly shows facet joint hypertrophy, osteophytes, calcification, and the degree of neural foraminal narrowing. CT is particularly useful for surgical planning.
MRI (Magnetic Resonance Imaging): MRI is the gold standard for evaluating facet hypertrophy and its effects on surrounding structures. It shows:
- The degree of facet joint enlargement
- Cartilage breakdown and joint inflammation
- Ligamentum flavum thickening
- Disc degeneration
- Neural compression
- Facet joint cysts, if present
Diagnostic Injections
Because imaging alone cannot definitively identify the facet joints as the source of pain, diagnostic injections can help confirm facet-mediated pain.
Medial branch blocks (MBB): These involve injecting local anesthetic near the medial branch nerves that supply the facet joint. If the injection provides significant pain relief (typically defined as 50-80% or more), it confirms that the facet joint is a significant pain generator.
Intra-articular facet joint injections: These involve injecting directly into the facet joint itself. However, recent research suggests that medial branch blocks may be more reliable for diagnostic purposes.
The two-block protocol: Many pain specialists perform two separate diagnostic blocks on different days. If both provide substantial pain relief, it strongly confirms that the facet joint is the source of the pain. A 2024 study examining diagnostic protocols found that, while controversial, properly performed diagnostic blocks improve the outcomes of subsequent treatments, such as radiofrequency ablation.8
Differential Diagnosis
It’s essential to rule out other conditions that can cause similar symptoms:
- Herniated disc with nerve root compression
- Sacroiliac joint dysfunction
- Myofascial pain syndrome
- Hip osteoarthritis (which can refer pain to the lower back)
- Compression fractures
- Infections (septic arthritis, though rare)
- Tumors
- Systemic inflammatory conditions
Conservative Treatment Options
Most patients with facet hypertrophy begin treatment with conservative, non-surgical approaches. These methods aim to reduce pain, improve function, and slow the progression of degeneration.
Medications
Nonsteroidal anti-inflammatory drugs (NSAIDs): Medications like ibuprofen and naproxen help reduce inflammation and pain. They work best when used regularly during flare-ups rather than only when pain is severe.
Acetaminophen: This pain reliever can be helpful for mild to moderate pain, particularly when combined with other treatments.
Muscle relaxants: Medications such as cyclobenzaprine or methocarbamol can help reduce muscle spasms that often accompany facet joint pain.
Topical treatments: Creams containing capsaicin, lidocaine, or NSAIDs can provide localized pain relief with fewer systemic side effects.
Important note: While opioid medications may provide short-term relief for acute pain, they are not recommended for long-term management of chronic facet joint pain due to risks of dependence and limited long-term effectiveness.
Physical Therapy
A well-designed physical therapy program is one of the most effective conservative treatments for facet hypertrophy. An evidence-based program should include:
Core strengthening: Building strength in the abdominal and back muscles provides better support for the spine, reducing stress on facet joints.
Hip and gluteal strengthening: Strong hip muscles, particularly the gluteus medius and maximus, help maintain proper spinal alignment and reduce compensatory stress.
Flexibility training: Gentle stretching of tight muscles, particularly hip flexors and hamstrings, can improve movement patterns and reduce strain on the lower back.
Postural training: Learning proper body mechanics for daily activities helps minimize facet joint stress.
Manual therapy: Hands-on techniques by a physical therapist can help improve joint mobility and reduce muscle tension.
A 2023 study found that when combined with facet joint injections, physical therapy significantly enhanced pain relief and functional improvement.1
Activity Modification
Avoiding positions and activities that aggravate pain while gradually building tolerance:
- Limit prolonged standing or walking
- Take frequent breaks to change position
- Avoid excessive spine extension and rotation
- Use proper lifting techniques
- Modify work stations for better ergonomics
Weight Management
For overweight individuals, losing even 5-10% of body weight can significantly reduce the mechanical load on facet joints and improve symptoms.
Injection Therapies
When conservative treatments provide insufficient relief, several injection options may be considered:
Facet joint injections: Injecting corticosteroid and local anesthetic directly into the joint can reduce inflammation and provide pain relief lasting weeks to months.
Medial branch blocks: These can provide both diagnostic information and therapeutic relief, typically lasting several weeks.
Newer biological therapies: Recent research has explored platelet-rich plasma (PRP) injections for facet joint pain. A 2025 systematic review found that PRP demonstrated superior long-term outcomes compared to corticosteroid injections, with one study showing an 80.96% success rate at 6 months with PRP versus diminishing effectiveness with steroids.1
When Conservative Treatment Isn’t Enough
Despite appropriate conservative care, some patients continue to experience significant pain and functional limitations. Recognizing when it’s time to consider more advanced treatments is important.
Signs Conservative Treatment Has Failed
Persistent pain despite 3-6 months of appropriate treatment: If you’ve faithfully followed a comprehensive conservative treatment plan without adequate improvement, additional interventions may be warranted.
Progressive neurological symptoms: Increasing weakness, numbness, or bowel/bladder dysfunction requires prompt evaluation.
Significant impact on quality of life: If pain prevents you from working, enjoying activities, sleeping, or caring for yourself despite conservative treatment, it’s time to explore other options.
Diminishing returns from injections: If diagnostic medial branch blocks confirmed facets as the pain source but therapeutic injections provide only brief relief, more definitive treatment may be needed.
Radiofrequency Ablation: A Proven Option
For patients who obtain good but temporary relief from diagnostic medial branch blocks, radiofrequency ablation (RFA) is an established treatment with strong evidence supporting its effectiveness.
How Radiofrequency Ablation Works
RFA uses heat generated by radiofrequency energy to create a controlled lesion on the medial branch nerves that carry pain signals from the facet joint. This interrupts the pain pathway without affecting motor function.
The procedure is performed under fluoroscopic (X-ray) guidance. A specialized needle is positioned near the target nerve, and radiofrequency energy heats the nerve to 80-85°C, creating a small lesion that disrupts pain signal transmission.
A Safer RFA Alternative
The Deuk Plasma Rhizotomy® procedure, developed at the Deuk Spine Institute, is a safer, more minimally invasive alternative to RFA. It's a 10 minute procure that utilizes cutting-edge plasma technology. The equipment enables the surgeon to operate with higher precision, removing only intended materials. Whereas RFA, uses a wider radius, carrying the risk of burning surrounding tissues.
When to Consider Surgical Consultation
In certain circumstances, surgical intervention may be necessary:
Severe spinal stenosis: When facet hypertrophy causes significant narrowing of the spinal canal or neural foramina, leading to progressive neurological deficits, surgery may be the best option.
Failed radiofrequency ablation: If RFA doesn’t provide adequate relief or relief is very short-lived, surgical decompression may be needed.
Unstable spondylolisthesis: When facet joint degeneration has led to significant spinal instability, fusion may be necessary.
Facet joint cysts with nerve compression: Large synovial cysts arising from facet joints may require surgical removal if they cause significant nerve compression.
If you’re considering surgical options or want a second opinion on your current treatment plan, Deuk Spine Institute offers free consultations and MRI reviews to help you understand all your options.
Surgical Treatment Options
When conservative treatments and less invasive procedures have been exhausted, surgery may be necessary to relieve pain and prevent further neurological deterioration.
Surgical Goals
The primary goals of surgery for facet hypertrophy are:
- Decompress neural structures (nerves or spinal cord)
- Remove sources of pain
- Stabilize the spine if instability is present
- Preserve as much normal anatomy and function as possible
Traditional Surgical Approaches
Laminectomy: This procedure involves removing a portion of the lamina (the back part of the vertebra) to create more space for the spinal cord and nerve roots. When facet hypertrophy contributes to spinal stenosis, a laminectomy with partial facetectomy (removal of part of the enlarged facet joint) may be performed.
Foraminotomy: This surgery enlarges the neural foramen where nerve roots exit the spinal canal. It may involve removing bone spurs and portions of hypertrophied facet joints that compress the nerve. For more information, see our guide on foraminotomy procedures.
Spinal fusion: In cases where facet joint removal creates instability or when significant instability already exists, spinal fusion may be necessary. This involves permanently joining two or more vertebrae together using bone grafts and hardware.
Minimally Invasive Approaches
Advances in surgical technology have enabled many decompression procedures to be performed through smaller incisions with less tissue disruption.
Endoscopic decompression: Using a small endoscope and specialized instruments, surgeons can remove enlarged facet joints and decompress nerves through incisions as small as one centimeter. This approach reduces muscle damage, blood loss, and recovery time.
Recent research comparing endoscopic neurotomy to percutaneous radiofrequency ablation found that while both techniques provided short-term pain relief, endoscopic neurotomy appeared to offer more durable long-term results.10
Considerations at Deuk Spine Institute
At Deuk Spine Institute, our approach prioritizes preservation of your natural spinal structures whenever possible. For patients with facet hypertrophy causing stenosis, we offer advanced endoscopic techniques that can:
- Remove only the portions of the facet joint causing compression
- Preserve spinal stability
- Minimize tissue trauma
- Enable same-day or next-day discharge
- Facilitate faster recovery
For patients whose primary problem is disc degeneration leading to facet overload, our Deuk Laser Disc Repair® procedure can address the underlying disc problem, potentially reducing stress on facet joints.
Making the Decision
Surgery should be considered when:
- You’ve exhausted appropriate conservative treatments
- Your quality of life is significantly impacted
- You have progressive neurological symptoms
- Imaging clearly shows nerve compression correlating with symptoms
- You understand the risks and benefits
We encourage patients considering surgery to seek expert evaluation and, when appropriate, a second opinion. Our team at Deuk Spine Institute offers free virtual consultations and MRI reviews to help you understand whether you’re a candidate for minimally invasive treatment.
Recovery and Prognosis
The long-term outlook for patients with facet hypertrophy depends on several factors, including the severity of degeneration, the treatment chosen, and individual patient factors.
What to Expect from Conservative Treatment
Timeline: Most patients who respond to conservative treatment notice improvement within 6-8 weeks, with continued gains over 3-6 months.
Realistic expectations: Conservative treatment typically doesn’t eliminate all pain but should reduce it to manageable levels and improve function. Complete elimination of symptoms is uncommon because the underlying joint degeneration remains.
Maintenance: Continuing exercises, maintaining a healthy weight, and using proper body mechanics are essential for long-term success.
What to Expect from Radiofrequency Ablation
Immediate results: Some patients notice improvement within days, though full benefit may take 2-3 weeks as inflammation from the procedure resolves.
Duration: Most patients experience 6-12 months of significant pain relief. Some experience benefits last 2 years or longer.
Repeatability: The procedure can be safely repeated when pain returns, often with continued good results.
Functional improvement: Beyond pain reduction, studies show improvements in sleep quality, walking ability, and reduced reliance on pain medications.9
What to Expect from Surgery
Recovery timeline varies by procedure:
- Minimally invasive endoscopic procedures: Return to light activities in 2-3 weeks, full recovery in 6-8 weeks
- Traditional open procedures: Return to light activities in 4-6 weeks, full recovery in 3-6 months
- Fusion procedures: Protected recovery period of 3 months, full recovery 6-12 months
Success rates: When patients are properly selected, surgical decompression for stenosis caused by facet hypertrophy has good to excellent outcomes in 70-90% of cases.
Long-term considerations: Some studies suggest that removing facet joints may increase stress on adjacent levels, potentially accelerating degeneration at those levels. This is one reason why minimally invasive techniques that preserve as much normal anatomy as possible may offer advantages.
Factors Affecting Prognosis
Age: Younger patients generally have better recovery potential, though older patients can also achieve excellent results with appropriate treatment.
Overall health: Conditions like diabetes, obesity, and smoking can impair healing and affect outcomes.
Psychological factors: Depression, anxiety, and pain catastrophizing are associated with poorer outcomes regardless of the treatment chosen.
Litigation/disability status: Patients involved in litigation or seeking disability tend to have poorer outcomes across all treatment types.
Treatment compliance: Patients who actively participate in rehabilitation and follow medical advice tend to have better outcomes.
Living with Facet Hypertrophy
For many patients, facet hypertrophy is a chronic condition that requires ongoing management. Keys to long-term success include:
- Maintaining core strength and flexibility
- Using proper body mechanics
- Managing weight
- Staying active while avoiding aggravating activities
- Using treatments (medications, injections) strategically during flare-ups
- Regular follow-up with healthcare providers
Etiology and Risk Factors
Spondylosis, or spine degeneration, is the leading cause of facet joint diseases. Osteoarthritis is the result of natural wear and tear. This process involves cytokines as well as proteolytic enzymes. Finally, facet hypertrophy happens by trauma from falls, sports injuries, or car accidents.
Facet hypertrophy occurs with inflammation of the synovium. Ankylosing and rheumatoid arthritis are two conditions that can cause inflammation of the synovial fluid. Spondylolisthesis is a condition that causes instability of the spine and may contribute to facet hypertrophy. Subluxation of the facet joint may also occur.
Some of the risk factors for facet arthritis include.
- Advanced age
- Degenerative disc disease
- Previous history of trauma or injury
- History of poor posture
- Family history of degenerative arthritis
Frequently Asked Questions (FAQs)
Q: Can facet hypertrophy be reversed or cured?
A: No, facet hypertrophy cannot be reversed. The enlargement of the joints and formation of bone spurs are permanent structural changes. However, treatments can effectively manage symptoms, improve function, and in many cases, provide substantial pain relief. The goal is not to cure the condition but to manage it effectively, so it has minimal impact on your quality of life.
Q: How do I know if my back pain is from facet hypertrophy or a herniated disc?
A: This can be challenging to determine solely from symptoms, as both conditions can cause lower back pain. However, there are some distinguishing features:
- Facet pain is typically worse with extension (bending backward) and rotation, while disc pain is often worse with flexion (bending forward)
- Facet pain tends to cause referred pain that doesn’t follow a specific nerve distribution, while disc herniations with nerve compression cause dermatomal pain (following a specific nerve path)
- Morning stiffness is more characteristic of facet arthritis
- Accurate diagnosis requires imaging (MRI) and often diagnostic injections
Q: Will I need surgery for facet hypertrophy?
A: Most patients with facet hypertrophy do not require surgery. Research shows that the majority of patients find adequate relief through conservative treatments like physical therapy, medications, and activity modification. For those who don’t respond to conservative care, radiofrequency ablation is often highly effective.
Surgery is typically reserved for cases where:
- Facet hypertrophy causes significant nerve compression (stenosis) with progressive neurological symptoms
- Conservative treatments and radiofrequency ablation have failed
- Quality of life is severely impacted
Even in these cases, many patients are candidates for minimally invasive procedures rather than traditional open surgery.
Q: Is radiofrequency ablation permanent?
A: Radiofrequency ablation provides long-lasting but not permanent relief. The procedure creates a controlled injury to the nerve that transmits pain signals from the facet joint. Over time (typically 6-12 months to 2 years), the nerve may regenerate, and pain can return. However, the procedure can be safely repeated with continued good results. Many patients go through cycles of ablation as needed, experiencing years of cumulative pain relief.
Q: Can exercise make facet hypertrophy worse?
A: The right exercises, properly performed, will not make facet hypertrophy worse and can actually improve symptoms by strengthening supporting muscles and improving flexibility. However, certain movements can aggravate facet joint pain:
Avoid: Deep back extension, heavy twisting, high-impact activities during flare-ups, exercises that cause pain
Beneficial: Core strengthening, hip strengthening, low-impact aerobic exercise (walking, swimming), flexibility work
Working with a physical therapist who understands facet joint conditions is important for developing an appropriate exercise program.
Q: Does facet hypertrophy always cause pain?
A: No. Research shows that many people have radiologic evidence of facet joint degeneration and hypertrophy on imaging studies without experiencing any pain. The mere presence of facet hypertrophy on an MRI or CT scan does not mean it’s causing your symptoms. This is why diagnostic injections are considered the gold standard for determining whether facet joints are the actual source of pain.
Q: Can facet hypertrophy cause leg pain?
A: Yes, but through different mechanisms. Facet joints can refer pain to the buttocks, hips, and upper thighs in a non-specific pattern. Additionally, when facet hypertrophy is severe enough to cause spinal stenosis, it can compress nerve roots, leading to radicular leg pain, numbness, or weakness that follows a specific nerve distribution. This is different from the referred pain pattern.
Q: What lifestyle changes can help manage facet hypertrophy?
Several lifestyle modifications can reduce symptoms:
- Maintain a healthy weight to reduce stress on facet joints
- Practice good posture during daily activities
- Use proper lifting techniques
- Take frequent breaks during prolonged standing or sitting
- Stay physically active with low-impact exercises
- Avoid smoking, which impairs healing and accelerates degeneration
- Manage stress, which can increase muscle tension and pain perception
- Get adequate sleep, which is essential for pain management
Q: Is facet hypertrophy a disability?
Facet hypertrophy itself is a medical diagnosis, not a disability determination. Whether it constitutes a disability depends on how significantly it impacts your ability to work and perform daily activities. Some people with facet hypertrophy have minimal symptoms and no functional limitations, while others have severe, persistent pain that significantly limits their activities. Disability determinations are made on a case-by-case basis, considering symptom severity, treatment response, and functional limitations.
Take Action: Your Next Steps
If you’re experiencing symptoms that may be related to facet hypertrophy, here’s your action plan:
If You Haven’t Been Diagnosed
- See a healthcare provider for proper evaluation, including physical examination and medical history.
- Get appropriate imaging, such as an MRI, to identify the source of your pain and rule out other conditions.
- Consider diagnostic injections if imaging shows facet joint problems, but it’s unclear whether they’re causing your symptoms.
If You’ve Been Diagnosed and Are Starting Treatment
- Commit to conservative treatment for at least 3 months before considering more invasive options. This includes physical therapy, prescribed medications, and activity modification.
- Work with a physical therapist experienced in treating spinal conditions. Follow your exercise program consistently.
- Track your symptoms using a pain diary to objectively assess whether treatments are helping.
- Make necessary lifestyle changes, including weight management, posture improvement, and ergonomic modifications.
If Conservative Treatment Has Failed
- Discuss radiofrequency ablation with your pain management specialist if diagnostic blocks confirm that facet joints are the source of your pain.
- Consider a second opinion if you’re being offered surgery. Understanding all your options is essential before making a major treatment decision.
- Get expert evaluation to ensure accurate diagnosis and explore minimally invasive alternatives to traditional surgery.
Get a Second Opinion
At Deuk Spine Institute, we understand that facet hypertrophy and related spinal conditions can be complex. Dr. Ara Deukmedjian personally reviews cases to provide expert guidance on diagnosis and treatment options.
We offer free virtual consultations and MRI reviews to help you:
- Understand what your imaging actually shows
- Determine whether your symptoms match your imaging findings
- Learn about all available treatment options
- Make informed decisions about your spine care
Schedule Your Free Virtual Consultation and MRI Review
Whether you’re just starting your journey with facet hypertrophy or have been struggling with chronic pain for years, expert evaluation can help ensure you’re on the right treatment path.
Different Diagnosis
When diagnosing facet hypertrophy, it is essential to rule out any other causes of back and neck pain.
- Rheumatoid arthritis
- Osteophytes (bone spurs)
- Myofascial pain
- Herniated discs
- Compression fractures
- Lumbar Radiculopathy
- Osteoarthritis of the hip
- Sciatica
- Impingement of the sacroiliac joint
- Synovial and ganglion cysts
- Ankylosing Spondylitis This type of arthritis can cause the vertebrae and joints to fuse, resulting in severe pain.
- Septic arthritis (this rare and infectious condition is more common in patients older than 60)
- Benign bone tumors
- Cancer
About the Author
Dr. Ara Deukmedjian, MD, is a board-certified neurosurgeon specializing in minimally invasive endoscopic spine surgery. He completed his neurosurgery residency at the University of Florida and has performed over 2,000 endoscopic spinal procedures. Dr. Deukmedjian has published extensively on advanced spine surgery techniques in peer-reviewed journals and serves as the Medical Director of Deuk Spine Institute in Melbourne, Florida. His approach emphasizes preserving natural spinal structures whenever possible while achieving excellent patient outcomes.
Medical review process: This article was written by Dr. Deukmedjian based on current peer-reviewed medical literature and 15+ years of clinical experience treating spinal conditions. Information is updated regularly to reflect the latest evidence-based treatment approaches.
Disclaimer: This article is for educational and informational purposes only and does not constitute medical advice. Individual patient outcomes vary based on numerous factors. Always consult with a qualified healthcare provider for diagnosis and treatment recommendations specific to your condition. If you experience severe pain, progressive neurological symptoms, or any emergency warning signs such as loss of bowel or bladder control, seek immediate medical attention.
Sources
1: https://pmc.ncbi.nlm.nih.gov/articles/PMC11703435/
2: https://www.ncbi.nlm.nih.gov/books/NBK493233/
3: https://pmc.ncbi.nlm.nih.gov/articles/PMC10764212/
4: https://www.ncbi.nlm.nih.gov/books/NBK541049/
5: https://deukspine.com/blog/foraminal-narrowing-symptoms-advanced-treatments
6: https://deukspine.com/blog/canal-stenosis
7: https://pmc.ncbi.nlm.nih.gov/articles/PMC10764212/